A 24-year-old contact lens wearer with unilateral vision loss requiring penetrating keratoplasty
Digital Journal of Ophthalmology 2019
Volume 25, Number 2
June 30, 2019
DOI: 10.5693/djo.03.2019.06.001
Volume 25, Number 2
June 30, 2019
DOI: 10.5693/djo.03.2019.06.001
Download PDF
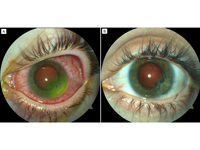
Figure 1
A, Dense corneal infiltrate with conjunctival injection at presentation. B, Clear corneal graft 9 weeks after penetrating keratoplasty. Best-corrected visual acuity was 20/40.
A, Dense corneal infiltrate with conjunctival injection at presentation. B, Clear corneal graft 9 weeks after penetrating keratoplasty. Best-corrected visual acuity was 20/40.
Seven days following admission, visual acuity in the left eye deteriorated to counting fingers. Examination revealed a 2.0 × 2.0 mm corneal perforation. A 4.0 mm Tenon’s capsule patch graft was applied under general anesthesia. Three days postoperatively, visual acuity remained unchanged, and there was interval development of 4+ anterior chamber inflammation and a small hypopyon. Anterior chamber paracentesis was performed, with injections of intracameral and intrastromal voriconazole (50 μg/0.1 mL) as well as intracameral amphotericin B (5 μg/0.1 mL). Oral voriconazole was increased to 300 mg twice daily after consultation with the Infectious Diseases unit.
Isolates from the corneal biopsy grew olivaceous green colonies consistent with Metarhizium anisopliae after 10 days at 25° C on potato dextrose agar (Figure 2). Minimum inhibitory concentrations of several antifungal drugs were determined (Table 1).
Seventeen days following admission, the corneal glue patch dislodged. A 5.5 mm peripheral therapeutic penetrating keratoplasty was performed, with repeat intracameral, intrastromal, and subconjunctival voriconazole injections (50 μg/0.1 mL). A small iridectomy was performed where iris tissue was adherent to the perforation site.
Postoperative assessments were satisfactory with a clear graft and quiet anterior chamber. On discharge, the patient was commenced on topical cyclosporine A 1% drops 4 times daily and continued on her regular dose of topical and systemic voriconazole. The eye remained quiet; hence, topical dexamethasone 0.1% drops 4 times a day was introduced on day eleven post-keratoplasty for prevention of rejection. A 5-week course of oral voriconazole was completed, and topical voriconazole was gradually weaned over 9 weeks (Figure 1B). Fifteen months after keratoplasty best-corrected visual acuity in the left eye was 20/20, with refraction of −3.50 −1.00 ×60, with no evidence of infective recurrence or graft rejection.
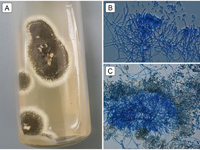
Figure 2
Metarhizium anisopliae strain isolated in the present case. A, Olivaceous-green colonies grown on potato dextrose agar at 25° C for 10 days. B, Specialized fungal stalks (conidiophores) aggregated in dense tufts with verticillate branching. C, Yellow-green cylindrical-shaped fungal spores (conidia), produced in long chains on conidiophores.
Metarhizium anisopliae strain isolated in the present case. A, Olivaceous-green colonies grown on potato dextrose agar at 25° C for 10 days. B, Specialized fungal stalks (conidiophores) aggregated in dense tufts with verticillate branching. C, Yellow-green cylindrical-shaped fungal spores (conidia), produced in long chains on conidiophores.
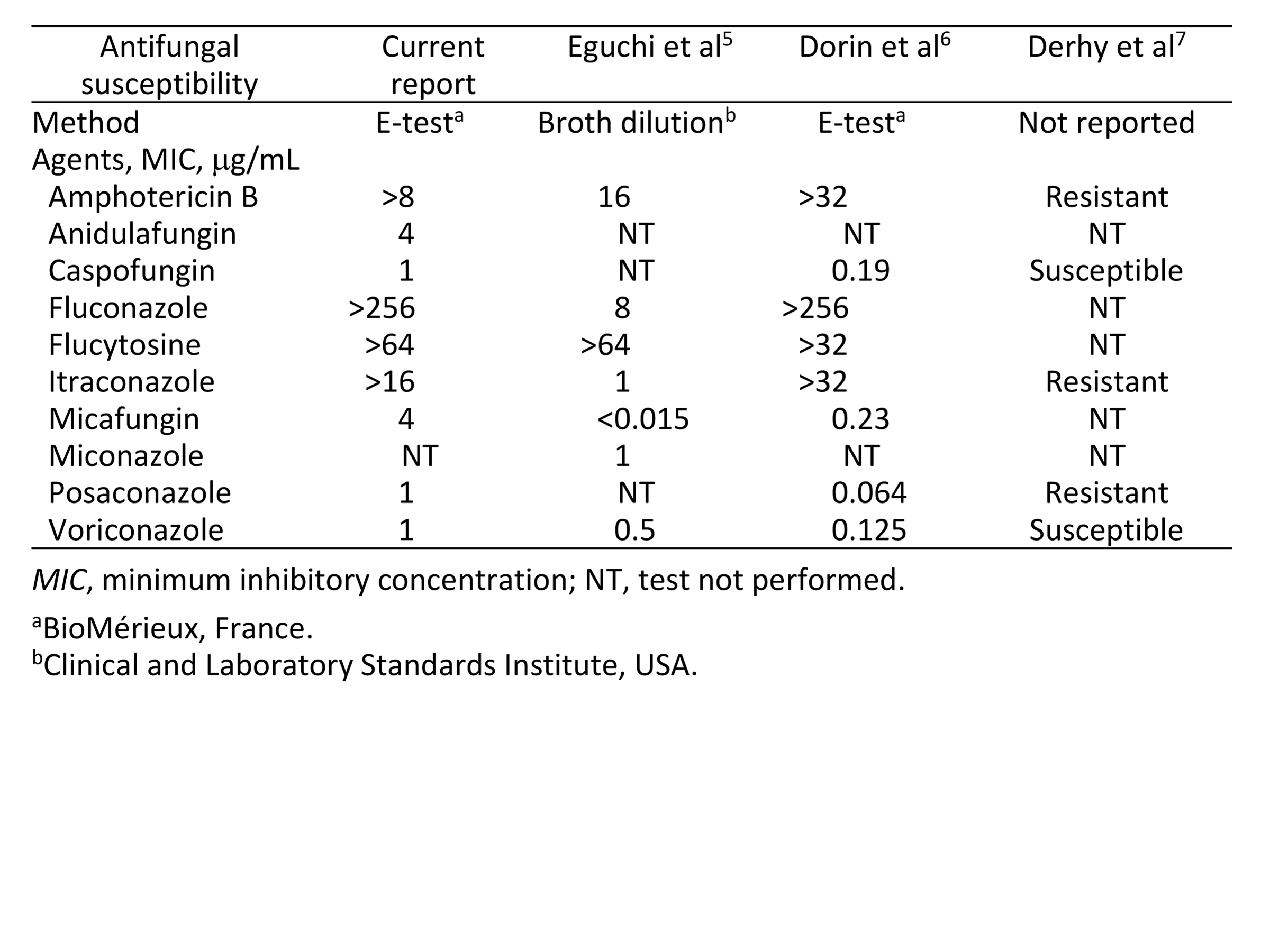
Table 1
Antifungal minimum inhibitory concentrations for ophthalmic isolates of Metarhizium anisopliae
Antifungal minimum inhibitory concentrations for ophthalmic isolates of Metarhizium anisopliae
Our search of the English-language literature yielded fewer than 10 reported cases of Metarhizium anisopliae ocular infection worldwide.(3-9) Mode of transmission typically involves agricultural exposure, with a history of vegetal trauma or soft contact lens wear. Although fungal keratitis is thought to be more common in tropical regions,(1) most published cases of Metarhizium anisopliae keratitis have arisen in temperate or extratropical climates, including Japan,(5) France,(6,7) the United States,(8) and Australia.(4) In this case, initial symptoms developed in Australia, but it is possible that the keratomycosis only became established on travel to Vietnam, which has a tropical climate and high relative humidity.
Management of filamentous fungal keratitis requires prompt identification through corneal scrapings or biopsy to aid directed therapy. The prognosis of Metarhizium anisopliae keratitis may be favorable with early administration of topical natamycin.(3,8,9) However, factors that contribute to poor visual outcomes include anterior chamber inflammation, large ulcer size, or scleral involvement.(4-7) In cases of deeper fungal invasion into the underlying corneal stroma, intraocular and systemic antifungals are recommended, and ideally tailored according to in vitro antifungal susceptibility testing.(1) Antifungal therapy should be maintained for at least 6 weeks, because negative scrapings during treatment may not exclude deep-seated fungal infection.
Surgical intervention may be required in up to 35% of patients with fungal keratitis refractory to maximal medical therapy.(10) Ideally, medical management should be provided to reduce the microbial burden, but surgery may be necessary in cases of progressive keratitis approaching the limbus or when perforation is imminent. The aim of surgery is to completely remove all infectious elements and involved tissue, and this may involve debridement, conjunctival flap, lamellar keratectomy, or penetrating keratoplasty, depending on the depth and severity of infection.(1,10) This may also include an iridectomy when the iris is involved. The poor surgical outcomes previously reported for Metarhizium anisopliae keratomycosis are likely attributable to advanced disease with associated scleral necrosis(4,5) or endophthalmitis(7) at the time of operation.
We report a case of Metarhizium anisopliae ocular infection with a favorable visual outcome following keratoplasty. Several reasons may account for the successful response in this patient, including the peripheral location of the infiltrate, aggressive targeted antifungal therapy (topical, intraocular, and systemic) based on isolate susceptibilities, and keratoplasty before scleral involvement. Fungal infections of the cornea are a challenging disease entity, and early recognition remains crucial to facilitate appropriate treatment and avoid potentially devastating outcomes.
Acknowledgments
The authors thank Drs. Helen Alexiou, Ian Ross, and Sarah Kidd, of the National Mycology Reference Centre, SA Pathology, Adelaide, South Australia, for their assistance with the microbiological identification, sensitivities, and sequencing.
2. Zimmermann G. Review on safety of the entomopathogenic fungus Metarhizium anisopliae. Biocontrol Sci Technol 2007;17:879-920.
3. De García MC, Arboleda ML, Barraquer F, Grose E. Fungal keratitis caused by Metarhizium anisopliae var. anisopliae. J Med Vet Mycol 1997;35:361-3.
4. Amiel H, Chohan AB, Snibson GR, Vajpayee R. Atypical fungal sclerokeratitis. Cornea 2008;27:382-3.
5. Eguchi H, Toibana T, Hotta F, Miyamoto T, Mitamura Y, Yaguchi T. Severe fungal sclerokeratitis caused by Metarhizium anisopliae: a case report and literature review. Mycoses 2015;58:88-92.
6. Dorin J, Debourgogne A, Zaïdi M, Bazard MC, Machouart M. First unusual case of keratitis in Europe due to the rare fungus Metarhizium anisopliae. Int J Med Microbiol 2015;305:408-12.
7. Derhy D, Sauer A, Sabou M, et al. Surgical treatment of Metarhizium anisopliae sclerokeratitis and endophthalmitis. Indian J Ophthalmol 2017;65:523-6.
8. Jani BR, Rinaldi MG, Reinhart WJ. An unusual case of fungal keratitis: Metarrhizium anisopliae. Cornea 2001;20:765-8.
9. Motley WW, Melson AT, Mortensen JE. Pediatric Metarrhizium anisopliae keratitis. J AAPOS 2011;15:101-3.
10. Xie L, Dong X, Shi W. Treatment of fungal keratitis by penetrating keratoplasty. Br J Ophthalmol 2001;85:1070-4.