A 45-year-old man with unilateral optic disc edema and vision loss
Digital Journal of Ophthalmology 2019
Volume 25, Number 1
March 29, 2019
DOI: 10.5693/djo.03.2019.02.002
Volume 25, Number 1
March 29, 2019
DOI: 10.5693/djo.03.2019.02.002
Download PDF
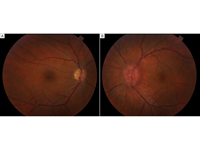
Figure 1
Initial fundus photographs demonstrating a normal posterior pole in the right eye and diffuse disc edema, dilation of the peripapillary vessels, and macular star in the left eye.
Initial fundus photographs demonstrating a normal posterior pole in the right eye and diffuse disc edema, dilation of the peripapillary vessels, and macular star in the left eye.
Magnetic resonance imaging (MRI) of the brain with and without contrast was obtained and revealed tram track enhancement of the left optic nerve sheath, with no white matter lesions or other abnormalities (Figure 3).
Additional studies were performed, including a lumbar puncture, which revealed normal cerebrospinal fluid constituents, negative cytology, and insufficient cells to perform flow cytometry. Whole-body PET computed tomography was also negative for signs of sarcoidosis or malignancy.

Figure 2
Initial Humphrey 30-2 SITA-fast automated visual field testing with scattered nonspecific loss in the right eye (B) and generalized depression with relative central sparing in the left eye (A).
Initial Humphrey 30-2 SITA-fast automated visual field testing with scattered nonspecific loss in the right eye (B) and generalized depression with relative central sparing in the left eye (A).
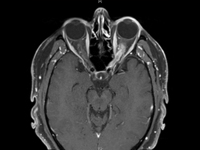
Figure 3
T1-weighted, post-contrast axial magnetic resonance imaging (MRI) of the brain demonstrating tram track enhancement of the left optic nerve sheath complex.
T1-weighted, post-contrast axial magnetic resonance imaging (MRI) of the brain demonstrating tram track enhancement of the left optic nerve sheath complex.
Thirty-three days following the initiation of steroids visual acuity improved to 20/30 in the left eye. MRI of the orbit with and without contrast performed at that time showed near resolution of the enhancement (Figure 4); 53 days following the initiation of steroids showed the disc edema and macular star in the left eye had resolved (Figure 5).
With taper of prednisone to 10 mg over the next 3 months, the patient’s visual acuity in the left eye declined to 20/40, requiring an increase in the steroid dose.
The patient was placed on monthly pulse intravenous cyclophosphamide for 3 months followed by oral daily azathioprine. Despite this immunomodulatory therapy, the patient was unable to be weaned from steroid therapy over the 2 years following initial presentation. At prednisone doses below 10 mg, he reported decreased vision in the left eye and demonstrated left optic nerve sheath enhancement on MRI. His condition remained exquisitely sensitive to steroids, with an increase in prednisone consistently effective in resolving his symptoms and MRI findings. The patient was switched to adalimumab, which facilitated discontinuation of corticosteroids. At his most recent visit, 6 months following initiation of adalimumab, the patient’s visual acuity was stable (20/25 in each eye), and the examination showed temporal pallor of the left optic nerve. Humphrey 30-2 SITA-Fast automated visual field showed a corresponding nasal defect in the visual field of the left eye (Figure 6).
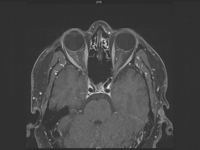
Figure 4
T1-weighted, post-contrast axial MRI of the orbit showing interval improvement in enhancement of the left optic nerve sheath complex.
T1-weighted, post-contrast axial MRI of the orbit showing interval improvement in enhancement of the left optic nerve sheath complex.
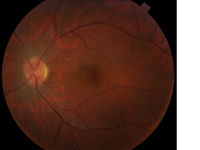
Figure 5
Fundus photograph of the left eye showing resolution in disc edema and macular star, with residual exudates in the nasal macula.
Fundus photograph of the left eye showing resolution in disc edema and macular star, with residual exudates in the nasal macula.

Figure 6
Final Humphrey 30-2 SITA-fast automated visual field testing with nasal defect in the left eye.
Final Humphrey 30-2 SITA-fast automated visual field testing with nasal defect in the left eye.
In this case, the initial findings prompted laboratory work-up for typical autoimmune or infectious causes of neuroretinitis, which was negative. An MRI of the brain was obtained to evaluate for a compressive lesion or evidence of infectious or autoimmune disease of the brain or orbit. The MRI study demonstrated tram track enhancement of the left optic nerve sheath. This finding shifted the differential diagnosis from neuroretinitis to optic perineuritis or optic nerve sheath meningioma. The subsequent clinical and radiological improvement with steroids was diagnostic of optic perineuritis rather than optic nerve sheath meningioma.
Optic perineuritis is characterized by inflammation of the optic nerve sheath and may be idiopathic or secondary to systemic disease, including Behçet disease, Crohn’s disease, granulomatosis with polyangiitis, giant cell arteritis, sarcoidosis, tuberculosis, syphilis, and metastasis.(6-13) The patient’s extensive studies as outlined above did not reveal an etiology.
Two reports in the literature have presented similar cases of idiopathic optic perineuritis with unilateral disc edema and a macular star.(14,15) Zhang et al reported a case involving enucleation because of pain and a concern for an optic nerve sheath meningioma; pathology demonstrated idiopathic optic perineuritis.(14) Wals et al. described a patient with a macular star, disc edema, and optic perineuritis who improved without treatment to baseline vision in 11 months; they presented the case as simultaneous optic perineuritis and neuroretinitis.(15) In the case described here, the partial macular star is incomplete and indicates secondary subretinal fluid and exudation from the primary inflammation of the optic disc and optic sheath. For the present case, the diagnosis of optic perineuritis with associated optic disc and macular edema is more appropriate than simultaneous optic perineurits and neuroretinitis.
This case highlights the importance of differentiating between optic neuritis and optic perineuritis, which is relevant clinically because of the similarity of presentation and difference in treatment (Table 1). Optic perineuritis and optic neuritis may be confused because patients with both diseases present with painful, monocular vision loss and disc edema. However, vision loss in optic perineuritis progresses over weeks, whereas in optic neuritis vision typically declines over the course of a few days. Long-term optic neuritis is associated with a 50% 15-year risk of developing multiple sclerosis (MS), while there is no known relationship between optic perineuritis and MS (7,16). Finally, MRI is crucial to differentiate the diseases. MRI primarily shows enhancement of the optic nerve itself in optic neuritis and in the nerve sheath in optic perineuritis.(7)
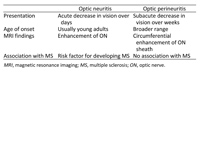
Table 1
Table 1. Differentiating optic neuritis and optic perineuritis(6)
Table 1. Differentiating optic neuritis and optic perineuritis(6)
2. Hoye VJ. Optical coherence tomography demonstrates subretinal macular edema from papilledema. Arch Ophthalmol 2001;119:1287.
3. Gittinger JW, Asdourian GK. Macular abnormalities in papilledema from pseudotumor cerebri. Ophthalmology 1989;96:192-4.
4. Leawit A, Morgenstern Z. Hypertensive retinopathy mimicking in a twelve-year-old girl. Surv Ophthalmol 1997;41:477-80.
5. Dreyer RF, Hopen G, Gass JD, Smith JL. Leber’s idiopathic stellate neuroretinitis. Arch Ophthalmol 1984;102:1140-5.
6. Purvin V. Optic perineuritis: clinical and radiographic features. Arch Ophthalmol 2001;119:1299.
7. Hickman SJ. Optic perineuritis. Curr Neurol Neurosci Rep 2016;16:16.
8. Liu KC, Chesnutt DA. Perineural optic nerve enhancement on magnetic resonance imaging in giant cell arteritis. J Neuroophthalmol 2013;33:279-81.
9. Liu TYA, Miller NR. Giant cell arteritis presenting as unilateral anterior ischemic optic neuropathy associated with bilateral optic nerve sheath enhancement on magnetic resonance imaging. J Neuroophthalmol 2015;35:360-3.
10. Yu-Wai-Man P, Crompton DE, Graham JY, Black FM, Dayan MR. Optic perineuritis as a rare initial presentation of sarcoidosis. Clin Experiment Ophthalmol 2007;35:682-4.
11. Jacob M, Kodjikian L, Ponceau B, Grange JD. La névrite péri-optique: complication méconnue de la tuberculose? Journal Français d’Ophtalmologie 2006;29:328.e1-328.e5.
12. Newman NJ, Grossniklaus HE, Wojno TH. Breast carcinoma metastatic to the optic nerve. Arch Ophthalmol 1996;114:102-3.
13. Yilmaz SG, Ture G, Zengin MÖ, et al. Optic nerve and dura mater involvement as the first sign of multiple myeloma. Eur J Ophthalmol 2015;25:77-9.
14. Zhang TL, Shao SF, Zhang T, et al. Idiopathic inflammation of optic nerve simulating optic nerve sheath meningioma: CT demonstration. J Comput Assist Tomogr 1987;11:360-1.
15. Wals KT, Ansari H, Kiss S, Langton K, Silver AJ, Odel JG. Simultaneous occurrence of neuroretinitis and optic perineuritis in a single eye. J Neuroophthalmol 2003;23:24-7.
16. Optic Neuritis Study Group. Multiple sclerosis risk after optic neuritis: final optic neuritis treatment trial follow-up. Arch Neurol 2008;65:727-32.