40 year old woman with a five-day history of visual loss in the right eye
Digital Journal of Ophthalmology 1997
Volume 3, Number 28
November 14, 1997
Volume 3, Number 28
November 14, 1997
PMHx: Ophthalmic Migraines
Meds: none
SHx: Non contributory
FHx: Non contributory
Color Plates:Normal color vision OU
Pupils: Equal, reactive, No APD
Amsler grid: no metamorphopsia OU
Visual Field: Confrontational visual fields demonstrated a large temporal scotoma in the right eye; the left eye was full to confrontation.
Motility: Full OU
Applanation pressure: 19 mmHg OD, 13 mm Hg OS
Slit lamp examination:normal anterior segments OU
Fundus examination: See Figures 1-3
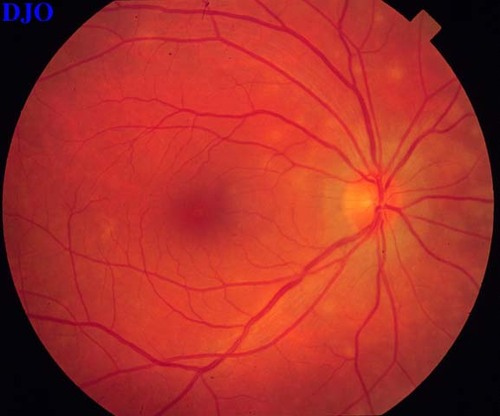
Figure 1
Figures 1-2. Ophthalmoscopy of the right eye revealed small, discrete white lesions at the level of the deep retina or retinal pigment epithelium scattered over the posterior pole. More lesions are noted nasally. The optic disc and macula were normal.
Figures 1-2. Ophthalmoscopy of the right eye revealed small, discrete white lesions at the level of the deep retina or retinal pigment epithelium scattered over the posterior pole. More lesions are noted nasally. The optic disc and macula were normal.
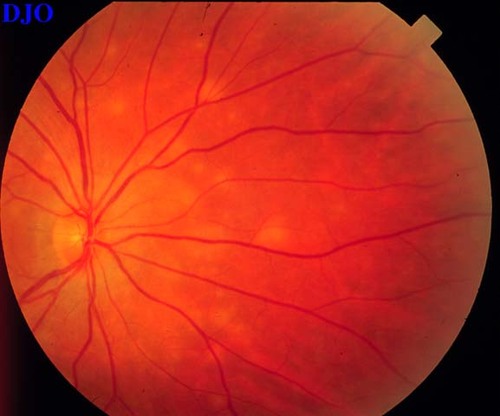
Figure 2

Figure 3
The left fundus was unremarkable
The left fundus was unremarkable
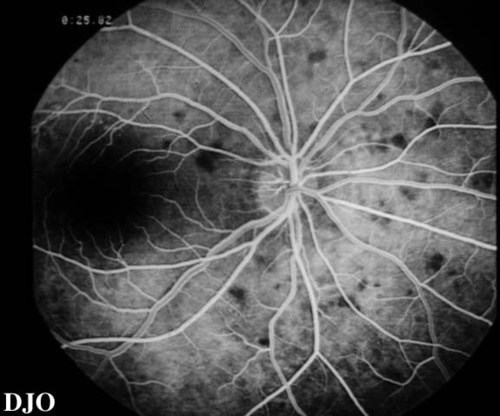
Figure 4
Shows early hypofluorescence of the lesions.
Shows early hypofluorescence of the lesions.
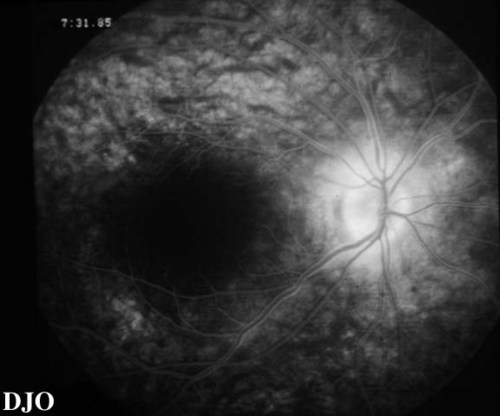
Figure 5
Shows late diffuse staining of the RPE and mild staining of the disc
Shows late diffuse staining of the RPE and mild staining of the disc
Features: Typically occurs in younger women, with frequent recovery of visual function and resolution of RPE lesions.
Noted on ophthalmoscopy: Lesions normally unilateral, multiple white dots are seen at the level of the deep retina or retinal pigment epithelium. The white dots are most prominent in the paramacular area, usually sparing the fovea.
Noted on fluorescein angiography: MEWDS lesions usually demonstrate early punctate hyperfluorescence and late staining corresponding to the location of the white dots and mild disc staining.
Acute posterior multifocal placoid pigment epitheliopathy (APMPPE)
Features: Transient visual loss in younger patients, with frequent recovery of visual function and resolution of RPE lesions. Usually bilateral involvement.
Noted on ophthalmoscopy: Usually bilateral, with considerably larger lesions than those associated with MEWDS which leave more obvious RPE alterations after fading
Noted on fluorescein angiography: APMPPE lesions block fluorescence early in the angiogram with late staining.
Acute retinal pigment epitheliitis
Features: Acute visual loss in younger patients, with near total visual recovery in 7-10 weeks.
Noted on ophthalmoscopy: Lesions appear as dark dots with surrounding halo of depigmentation; these spots become more pigmented with clinical recovery.
Noted on fluorescein angiography: Appear as hypofluorescent areas surrounded by hyperfluorescence.
Birdshot retinochoroidopathy
Features: Appears in older patients and is bilateral. Does not present with acute loss of vision.
Noted on ophthalmoscopy: Manifests as multiple cream-colored lesions at the level of the RPE or deeper. Frequently associated with cystoid macular edema, vitreous reaction, and retinal vascular leakage.
Noted on fluorescein angiography: Characteristically, reveals hypofluorescence in the early phase with slight diffuse hyperfluorescence in the late phase.
The patient was felt to have multiple evanescent white dot syndrome and was followed conservatively without treatment. The patient has since experienced a gradual improvement in her visual symptoms with a concomitant resolution of the white lesions.
MEWDS, first described in 1984, most commonly affects healthy younger women, as is true in this patient's case. Typically, patients present with rapidly progressive unilateral visual loss. Had formal visual field testing been performed, it is likely that an enlarged blind spot would have been demonstrated. Other characteristic clinical findings in MEWDS, which were not noted in this patient, include a granular appearance of the macula, optic disc edema, retinal vascular sheathing, and vitreal cells.
Although the cause of MEWDS remains unknown, ophthalmoscopic localization of the lesions to the deep retina and abnormal electroretinographic studies have pointed to a disorder of the retinal pigment epithelium which secondarily affects the adjacent photoreceptors. Fluorescein angiography is often a valuable tool in confirming a diagnosis of MEWDS in a patient with characteristic fundus findings. Interestingly, this patient did not display the typical early hyperfluorescent spots of MEWDS, but instead had hypofluorescent lesions, which are more characteristic of APMPEE. Although the fundoscopic appearance of the lesions was strongly suggestive of MEWDS, a recovery angiogram would be helpful in confirming the diagnosis; one would expect significantly less RPE alteration than is seen after resolution of APMPEE. Investigators have also suggested that indocyanine green angiography (ICG) may be a useful adjunct in the diagnosis of MEWDS, as it demonstrates a greater number of lesions than are seen with ophthalmoscopy or fluoroscein angiography.
MEWDS is usually a self-limited disorder, with resolution of symptoms and the white dots over a 4 to 6 week period. However, a chronic recurrent form of the disease has been described in which multiple recurrences have involved both eyes Additionally, multifocal choroiditis and choroidal neovascularization have been associated with MEWDS, as has persistent enlargement of the blind spot. Patients with acute idiopathic blind spot enlargement (AIBSE) without optic disc edema are likely a subgroup of patients with MEWDS who have rapid resolution of their fundoscopic abnormalities with a protracted enlargement of the blind spot. When these patients are examined after resolution of the white dot lesions and the characteristic fluorescein angiographic findings, the presentation is indistinguishable FROM AIBSE, suggesting that AIBSE may represent a variation of MEWDS.
2) Gass JDM: Acute posterior multifocal placoid pigment epitheliopathy. Arch Ophthalmol 1968;80:177-185.
3) Krill AE, Deutman AF: Acute retinal pigment epitheliitis. AM J Ophthalmol 1972;74:193-205.
4) Ryan SJ, Maumenee AE: Birdshot retinochoroidopathy. Am J Ophthalmol 1980;89:31-45.
5) Le D, Glaser BM, Murphy RP, Gordon LW, et al:Indocyanine green angiography in multiple evanescent white-dot syndrome. Am J Ophthalmol 1994;117:7-12.
6) Sieving PA, Fishman GA, Jampol LM, et al: Multiple Evanescent white dot syndrome: II. Electrophysiology of the photoreceptots during retinal pigment epithelial disease. Arch Ophthalmol, 1984; 102:675-679.
7) Tsai L, Jampol LM, Pollock SC, et al:Chronic recurrent multiple evanescent white dot syndrome. Retina 1994;14:160-163.
8) Callanan D, Gass DM: Multifocal choroiditis and choroidal neovascularization associated with the multiple evanescent white dot and acute idiopathic blind spot enlargement syndrome. Ophthalmol 1992;99:1678-1685.
9) Hamed LH, Glaser JS, Gass DM, et al: Protracted enlargement of the blind spot in multiple evanescent white dot syndrome. Arch Ophthalmol 1989;107:194-198.
10) Jampol LM: MEWDS, MFC, PIC, AMN, AIBSE, and AZOOR: one disease or many? [editorial]. Retina 1995;15:373-378.