22 year old female comes in for a normal eye exam
Digital Journal of Ophthalmology 1997
Volume 3, Number 27
October 21, 1997
Volume 3, Number 27
October 21, 1997
PMH: None.
Meds: None.
Social Hx: Non smoker, 1-2 cans of beer a day
Family Hx: Grandmother with cervical cancer and first cousin with renal cysts
Pupils: Normal OU
Motility: Full
External exam: Normal.
Slit lamp examination: Normal OU
Fundus examination: Normal OD
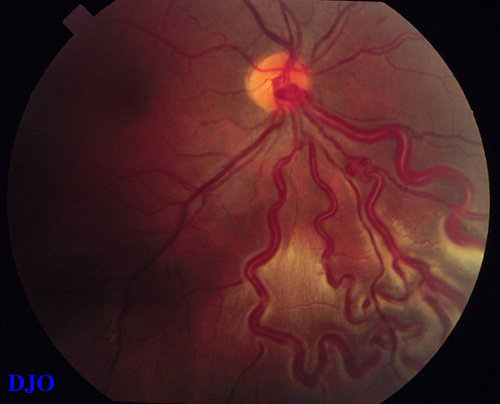
Figure 1
(OS) Large dilated vessels in the inferior quadrant.
(OS) Large dilated vessels in the inferior quadrant.
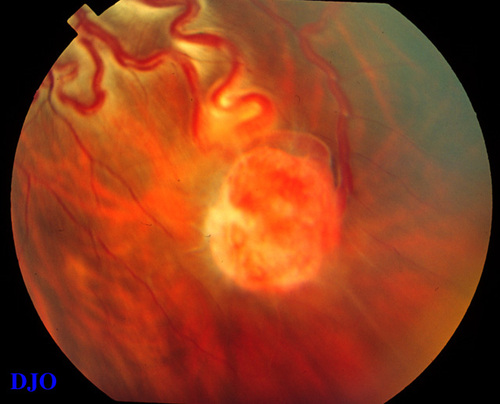
Figure 2
(OS) Vascular tumor in the inferior perophery with large feeder vessels.
(OS) Vascular tumor in the inferior perophery with large feeder vessels.
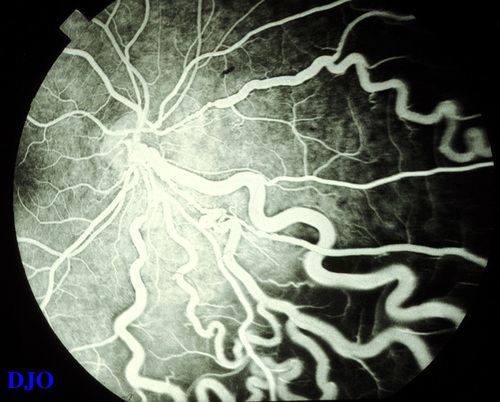
Figure 3
(OS) Fluorescein angiogram of the large dilated vessels.
(OS) Fluorescein angiogram of the large dilated vessels.
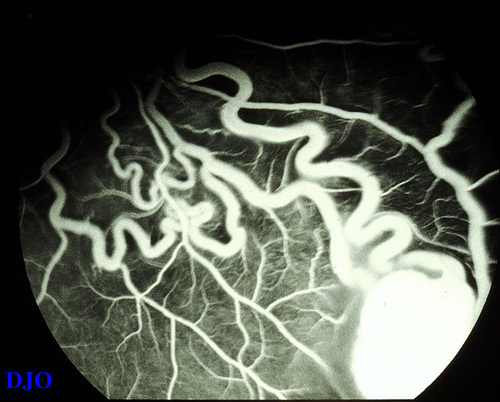
Figure 4
(OS) Fluorescein angiogram of the vascular tumor. It hyperfluoresces in the early phases and the feeder vessels fill. Aside FROM the feeder vessels, the surrounding vasculature appears normal.
(OS) Fluorescein angiogram of the vascular tumor. It hyperfluoresces in the early phases and the feeder vessels fill. Aside FROM the feeder vessels, the surrounding vasculature appears normal.
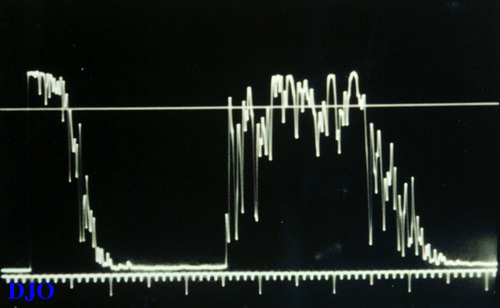
Figure 5
(OS) A-scan ultrasound of the lesion shows a 2.3 mm elevated mass with a medium to high reflectivity and a slightly irregular internal structure.
(OS) A-scan ultrasound of the lesion shows a 2.3 mm elevated mass with a medium to high reflectivity and a slightly irregular internal structure.
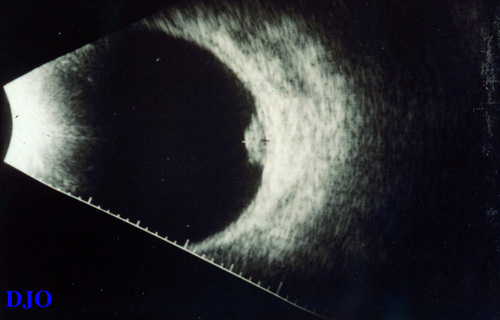
Figure 6
(OS) B-scan ultrasound of the lesion shows a slightly irregular highly reflective dome shaped lesion in the inferotemporal fundus extending to the equator.
(OS) B-scan ultrasound of the lesion shows a slightly irregular highly reflective dome shaped lesion in the inferotemporal fundus extending to the equator.
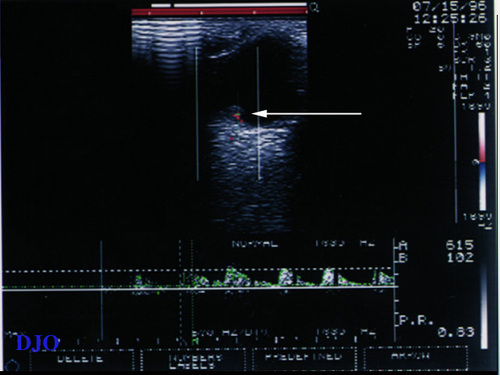
Figure 7
(OS) Color Doppler of the lesion (white arrow) shows minimal high flow vascularity in the lesion or the feeder vessels.
(OS) Color Doppler of the lesion (white arrow) shows minimal high flow vascularity in the lesion or the feeder vessels.
Congenital.
- Capillary retinal hemagiomas (Von Hippel tumor)
- Cavernous retinal hemangiomas
- Coat's disease ( Lebers miliary aneurysm)
Acquired
- Sickle cell retinopathy
- Uveitis
- Retinopathy of prematurity
- Chronic retinal detachment
- Acquired retinal hemagiomas
- Angiomatosis retinae with retinitis pigmentosa
Produces Large Dilated Vessels
- Arteriovenous aneurysm
- Racemose aneurysm( Wyburn-Mason)
History of von Hippel Tumors and the Lindau syndrome.
Von Hippel tumor was first described in 1904 by Eugene von Hippel a german ophthalmologist. (1) It wasn't until Arvid Lindau a Swedish pathologist noted the association between hemangiomatous cerebellar cysts and retinal hemangioblastomas that the von Hippel - Lindau disease was described. (2)
Von-Hippel Lindau disease is a rare familial cancer syndrome characterized by the development of retinal hemangioblastomas and infratentorial hemangioblastomas of the cerebellum, brainstem or spinal cord. Renal cell carcinoma, pheochromocytoma, and cysts of the kidney , pancreas, lungs, liver, bone and epididymus are also found in patients with this syndrome. The incidence is 1 in 36,000 births per year and is inherited in an autosomal dominant fashion with variable expression.
Retinal Hemangioblastomas
Retinal hemangioblastomas occur in up to 70% of patients with this syndrome by the age of 60. (3) These hemangioblastomas are usually found on routine exam of either patients with von-Hippel Lindau disease or their a symptomatic relatives. If untreated they can progress to the development of vitreous hemorrhage or retinal exudation which can result in retinal detachment, retinal membrane formation, and possible neovascular glaucoma.
There are two types of hemangioblastomas. The endophytic type is a raised vacular mass associated with large feeder vessels and occurs in most case in the periphery. This is the type of tumor our patient had. The exophytic type is usually juxtapapillary and is localized in the retinal layers.
Histopathology
The hemangioblastomas are made of capillary like vessels separated by large polygonal interstitial cells with a foamy cytoplasm. The foamy cytoplasm represents lipid deposition identified as cholesterol stearate. The cells are thought to be fibrous astrocytes.
Genetics
The gene has been positionally cloned to the short arm of chromosome 3 (3p25-p26). (4) (5) Several mutations have been identified including large germline mutations, as well as missense and nonsense deletions and insertions. The protein that is encoded is a 213 amino acid protein that binds to the B/C subunit of elongin. Elongin is a protein that increase the transcription rate of RNA polymerase II. The von Hippel Lindau (VHL) protein is a negative regulator of Elongin. A mutated VHL protein cannot negatively regulate elongin and allows for unchecked transcription of a particular gene. (6) (7) This is only one elucidated mechanism, work is still under way to understand this gene fully.
Treatment
Retinal hemangioblastomas can be treated with laser photocoagulation, cryotherapy and irradiation therapy. Proton beam irradiation has also proved a promising modality for larger more advanced hemangioblastomas.
2) Lindau A: Studien uber Kleinhirncysten: Bau, Pathogenese, und Beziehungen zur Angiomatosis Retinae. Acta Pathol Microbiol Scand 1(suppl):1,1926.
3) Maher ER, Yates JRW, Harries R, et al: Clinical feature and natural history of von Hippel - Lindau disease. Quart J Med 77:1151, 1990.
4) Pericak-Vance MA, Nunes KJ, Whisenant E, et al: Genetic mapping of dinucleotide repeat polymorphisms and VHL disease to 3p25-26. Am J Med Genetic 30:487, 1993.
5) Latif F, Tory K, Gnarra J, et al.: Identification of the von Hippel-Lindau disease tumor supressor gene. Science 260:1317, 1993.
6) Duan DR, Pause A, Burgess WH, et al.: Inhibition of transcription by the VHL tumor suppressor protein. Science 269:1402, 1995.
7) Kibel A, Iliopoulos O, Decaprio JA, et al.: Binding of the von Hippel-Lindau tumor suppressor protein to Elongin B and C. Science 269:1444, 1995.