25 year old kickboxer with progressive proptosis
Digital Journal of Ophthalmology 1997
Volume 3, Number 26
September 24, 1997
Volume 3, Number 26
September 24, 1997
PMH: Sinusitis
Meds: Biaxin
Social Hx: Kickboxing as a hobby
Family Hx: Negative
Pupils: Normal OU
Motility: Full without diplopia
Color: Normal OU
Visual Fields: Full OU
External exam: Figure 1
Slit lamp examination: Normal OU
Fundus examination: Normal OU

Figure 1
Mild left upper lid swelling temporally, slight resistance to retropulsion OS, 2 mm exophthalmos OS by Hertel, no sinus tenderness or palpable masses.
Mild left upper lid swelling temporally, slight resistance to retropulsion OS, 2 mm exophthalmos OS by Hertel, no sinus tenderness or palpable masses.
Pathology

Figure 2a
Orbital CT: Axial, showing an expansile soft tissue mass obliterating the greater wing of the sphenoid bone.
Orbital CT: Axial, showing an expansile soft tissue mass obliterating the greater wing of the sphenoid bone.

Figure 2b
Orbital CT: Coronal bone window, showing scalloping of the greater wing of the sphenoid bone indicating bony destruction.
Orbital CT: Coronal bone window, showing scalloping of the greater wing of the sphenoid bone indicating bony destruction.
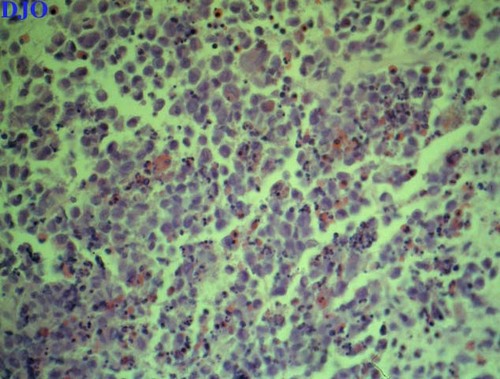
Figure 3
Histology revealed a number of large histiocytes with scattered eosinophills, lymphocytes and plasma cells.
Histology revealed a number of large histiocytes with scattered eosinophills, lymphocytes and plasma cells.
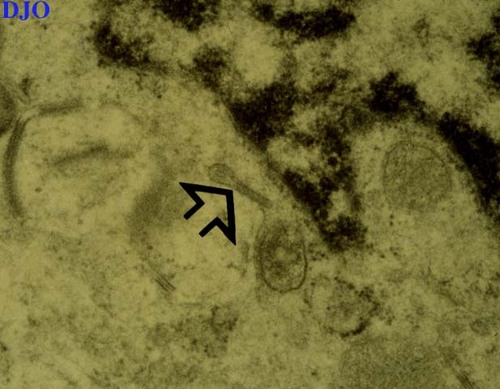
Figure 4
Electron microscopy demonstrated the presence of Birbeck granules (arrow) within a few of the histiocytes.
Electron microscopy demonstrated the presence of Birbeck granules (arrow) within a few of the histiocytes.
P. C. did extremely well following his excision and curettage. He experienced resolution of both his pain and proptosis. Repeat CT scan one and a half years after his surgery revealed regeneration of the involved bone, typically seen in these patients when the periosteum is preserved.
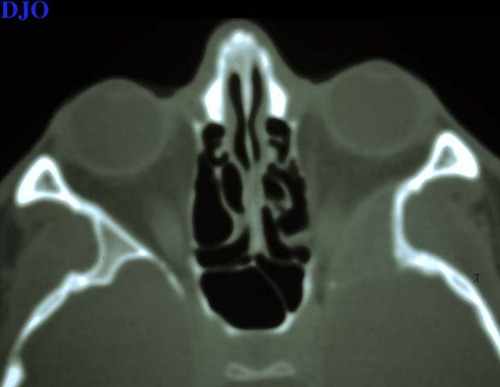
Figure 5a
Figures 5a-5b. Orbital CT prior to surgery.
Figures 5a-5b. Orbital CT prior to surgery.
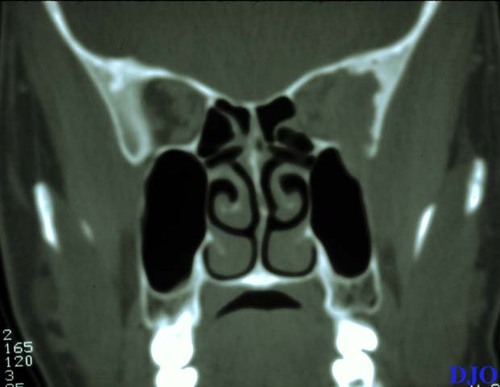
Figure 5b
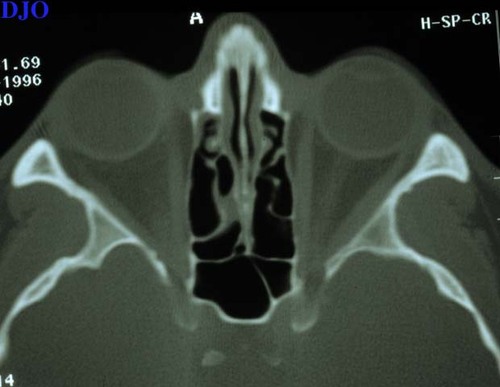
Figure 6a
Figures 6a-6b. Orbital CT one and a half years after surgery.
Figures 6a-6b. Orbital CT one and a half years after surgery.
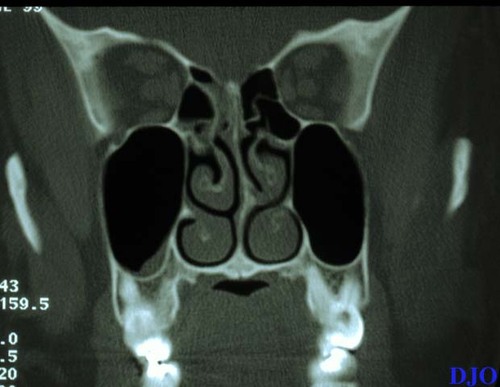
Figure 6b
Eosinophilic granuloma is considered to be a localized form of histiocytosis X or Langerhans' cell histiocytosis, a process which predominantly involves infants or children. It falls on the more benign aspect of a spectrum of disease which includes Hand-Schuller-Christian and Letterer-Siwe syndromes. The former is a chronic disseminated histiocytosis classically presenting with a triad of lytic skull lesions, proptosis, and diabetes insipidus. Letterer-Siwe syndrome is an acute virulent histiocytosis which can rapidly lead to death secondary to bone marrow and vital organ infiltration. In general, older patients such as the one presented here tend to have more localized disease with a better prognosis.
Orbital involvement is characterized by pain, lid swelling, and proptosis. Histiocytosis X accounts for less than 1% of all orbital tumors, but up to 24% of afflicted patients will demonstrate an orbital lesion. The process has a predilection for the superotemporal orbital rim. There is almost always bony disease when the process invades the orbit. Orbital disease is less common in the acute disseminated forms seen in infants. Intraocular involvement is rare, and papilledema with optic atrophy has been reported with intracranial histiocytosis.
As demonstrated by this case, histology typically reveals the presence of sheets of large histiocytes. These cells are a specific type of histiocyte known as Langerhans' cells. They possess prominent nucleoli with grooved or folded nuclei and stain positive for specific cell markers such as S-100 or OKT-6. On electron microscopy, Birbeck granules may be seen in about 2% of the histiocytes. These are rod or tennis racket shaped cytoplasmic inclusions which aid in diagnosis. Multinucleated giant cells and variable numbers of eosinophills, lymphocytes, and plasma cells are also present.
Patients need to be evaluated for other foci of disease when they present to the ophthalmologist. This patient underwent a radionuclide bone scan which revealed that the orbit was the only site of involvement, as would be expected based on his age. Liver and pulmonary function tests may also be of use in detecting widespread disease.
Localized forms of eosinophillic granuloma such as the case presented here have an excellent prognosis overall. Such forms may be treated by observation or by surgical excision with bone curettage if there is discomfort or functional or cosmetic compromise. Radiotherapy with doses ranging between 300-1000 cGy may be employed for larger lesions or if surgical access is particularly difficult. There have been case reports of resolution with intralesional steroid injection. Disseminated disease requires systemic therapy, starting with steroids and progressing to chemotherapeutic agents if there is inadequate response. In children under age two with disseminated disease, the five year survival is less than 50%.