20 year old woman with back pain, neck pain, and blurry vision OS
Digital Journal of Ophthalmology 1997
Volume 3, Number 25
September 7, 1997
Volume 3, Number 25
September 7, 1997
POHx: None
PMHx: The patient notes a history of "migraine" headaches which were frontal in location and which did not have a preference for one side of the head. Sometimes, the headaches were associated with nausea. The patient recalls two episodes of headache that were associated with vomiting.
Meds: Percocet, valium, robaxin, fioricet all prescribed since the onset of the patient's symptoms
SHx: Non-contributory
FHx: Non-contributory
Pupils: 2+ left afferent pupillary defect
External exam: Normal. 5'4" and 135 lbs
Motility: Full
Slit lamp examination: Normal ou. Anterior chambers deep and quiet.
Intraocular pressure: 16 mm Hg OU
Visual field Examination: See Figures 1-2
Fundus examination: See Figures 3-4
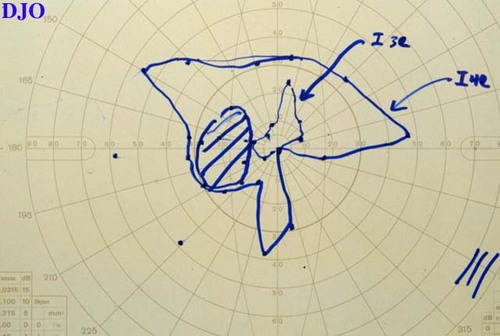
Figure 1
Figures 1-2. Goldmann visual fields are shown. In the left eye there is an enlarged blind spot and depression of the inferior visual field, particularly nasally. There is also constriction of the I4e and I3e isopters. In the right eye there is an enlarged blind spot and there is depression of the inferonasal visual field. There is also mild constriction of the I4e, I3e and I2e isopters.
Figures 1-2. Goldmann visual fields are shown. In the left eye there is an enlarged blind spot and depression of the inferior visual field, particularly nasally. There is also constriction of the I4e and I3e isopters. In the right eye there is an enlarged blind spot and there is depression of the inferonasal visual field. There is also mild constriction of the I4e, I3e and I2e isopters.
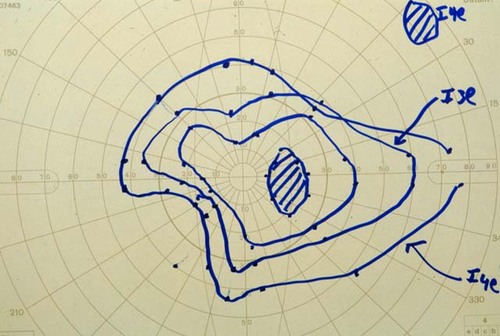
Figure 2

Figure 3
Figures 3-4. The right and left fundi are shown. Both the right and left fundi showed marked disk edema with blurred margins and tortuous retinal vessels.
Figures 3-4. The right and left fundi are shown. Both the right and left fundi showed marked disk edema with blurred margins and tortuous retinal vessels.

Figure 4

Figure 5
Figures 5-6. On the left is an axial T1 weighted MRI image which shows prominence of the optic disks, but which shows no masses present in the orbit. On the right is a coronal T1 weighted MRI image which shows small ventricles and an empty sella. Other than the above findings the MRI was normal with no evidence of tumor.
Figures 5-6. On the left is an axial T1 weighted MRI image which shows prominence of the optic disks, but which shows no masses present in the orbit. On the right is a coronal T1 weighted MRI image which shows small ventricles and an empty sella. Other than the above findings the MRI was normal with no evidence of tumor.
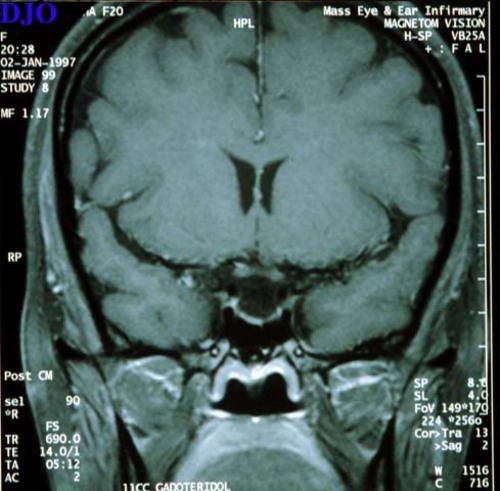
Figure 6
- Non-arteritic anterior ischemic optic neuropathy
- Arteritic anterior ischemic optic neuropathy
- Increased intracranial pressure (e.g. intracranial tumor, sagital sinus thrombosis, idiopathic intracranial hypertension, etc)
Because of the bilateral chronic appearing disk edema the patient was suspected to have increased intracranial pressure. When the MRI showed no mass lesions, idiopathic intracranial hypertension was felt to be the most likely cause of this patients signs and symptoms. This diagnosis was confirmed by a lumbar puncture which showed a CSF pressure of > 300 mm of water ( nl < 200 mm of water). The CSF composition was also found to be normal.
Epidemiology:
Pseudotumor cerebri can affect patients of any age including children. However, the peak age is in the third decade. Approximately 90% of patients are women and most patients are obese. (Our patient was only slightly obese)
Clinical Features:
Initial symptoms in this condition include severe headache and disturbances in vision. Patients may also complain of transient obscurations in their vision lasting seconds. Double vision may also occur as a result of an associated 6th nerve palsy due to increased intracranial pressure. Any other cranial nerve deficit or neurological problem would be highly unusual in pseudotumor cerebri and should make a clinician suspicious of the diagnosis. Decreased vision in the form of substantial visual field loss or decreased acuity may occur in the setting of advanced disease.
Diagnosis:
Diagnosis of this condition requires 1) increased intracranial pressure on lumbar puncture (>200 mm of water), 2) a "normal" head imaging scan (findings which can be seen in pseudotumor cerebri, but which are often considered within nomrla limits are small ventricles, an enlarged CSF sapce around the optic nerves, and an empty sella turcica) and 3) normal CSF composition
Management:
For obese patients, treatment begins with a weight control program since decreasing weight has been shown to decrease the intracranial pressure in this condition. Medical management generally consists of acetazolamide 500 mg to 2 gm P.O. qd. Furosemide and steroids are also occasionally used. When visual field loss occurs in the face of medical management or if there is significant visual field loss at presentation, optic nerve sheath fenestration is indicated. Not infrequently, unilateral optic nerve sheath fenestration may result in decrease of optic disk edema in both eyes.
Clinical Course:
Our patient underwent optic nerve sheath fenestration within 48 hours of her presentation because of her severe visual field loss and concern that she could lose her central acuity. Over the subsequent weeks her visual fields expanded substantially OU and showed marked decrease in her disk edema in both eyes.
2) Lessel S, Rosman NP: Permanent visual impairment in childhood pseudotumor cerebri. Arch Neurol 43:801 (1986)