23 year old man with a history of alcohol abuse
Digital Journal of Ophthalmology 1997
Volume 3, Number 24
August 15, 1997
Volume 3, Number 24
August 15, 1997
PMHx: none
Meds: none
SHx: History of alcohol abuse and cocaine abuse. He denies intravenous drug abuse
FHx: Non contributory
Hospital Course:
The patient was admitted to the medicine service and he was placed on broad spectrum antibiotics. His work-up was negative for infection. Several days INTO his admission the patient noted decreased vision and an ophthalmology consult was obtained.
Pupils: Equal, reactive, No APD
Slit lamp examination: normal anterior segments OU
Fundus examination: See Figures 1a-1b
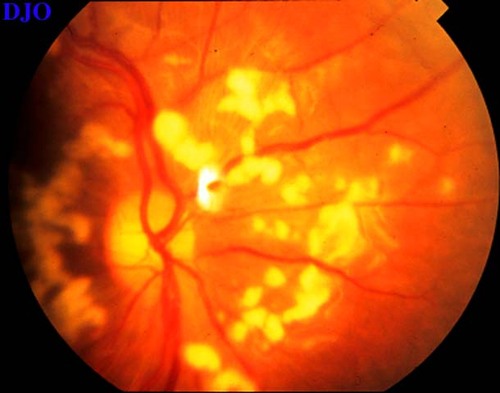
Figure 1a
Figures 1a-1b. Both fundi SHOW multiple large supericial cotton wool spots surrounding a normal looking optic nerve. A small intraretinal hemorrhage was also seen in the left eye.
Figures 1a-1b. Both fundi SHOW multiple large supericial cotton wool spots surrounding a normal looking optic nerve. A small intraretinal hemorrhage was also seen in the left eye.
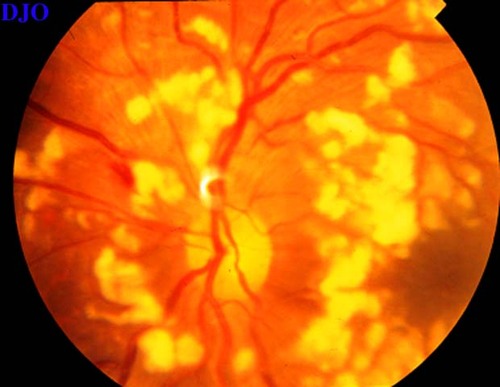
Figure 1b
- Hypertensive retinopathy
- Diabetic retinopathy
- Collagen vascular disease (e.g. lupus)
- Leukemia
- Anemia
- Purtschers retinopathy
- Valsalva retinopathy
This patient's fundus picture was typical for Purtscher's-like retinopathy. A careful review of the patient's history was done in an attempt to identify any recent trauma or other systemic disease which are known to be associated with Purtscher's retinopathy. No definite medical diagnosis was made. However, the patient did have an episode of severe nausea and vomiting two weeks prior to admission which was consistent with an episode of pancreatitis, but no further work-up had been done at that time.
Purtscher's retinopathy was first described by Otmar Purtscher a Tyrolean ophthalmologist. He described the retinal findings in this condition as consisting of cotton wool spots and retinal hemorrhages confined to the posterior pole in patients complaining of severe visual loss following head trauma. Similar findings were later described in the setting of acute pancreatitis, chest compression injuries, autoimmune disease, chronic renal failure, sexual abuse, retrobulbar anesthesia, and after complicated childbirth. Symptoms associated with this condition usually include sudden severe bilateral visual loss in the setting of extraocular trauma and bilateral central scotoma.
Several theories have been proposed regarding the pathogenesis of this condition. Purtscher himself believed that the retinal findings were an extension of cerebral edema following head trauma. The presence of this fundus picture in patients without head trauma have led to other theories including the possibility of air or fat emboli and increased intra-orbital pressure. Recently, a complement activation theory has been described which proposes that the conditions associated with Purtscher's-like retinopathy all activate C5 to C5a which in turn causes leukocytes to aggregate and form small leukocyte emboli.
Treatment with papaverine and high dose steroids have been described, but only in anecdotal fashion. The visual recovery varies FROM patient to patient with some recovering to near baseline vision.
2) Sandy-McCoy I, Morse P. Retinopathy associated with acute Pancreatitis. Am J Ophthalmol 100: 246-251, 1985
3) Kelley JS. Purtscher's retinopathy related to chest compression by Saftey belts Am J Ophthalmol 74: 278-283, 1972