38 year old myopic male with recurrent red eye OD
Digital Journal of Ophthalmology 1997
Volume 3, Number 21
June 14, 1997
Volume 3, Number 21
June 14, 1997
POHx: Recurrent red eye OD twice ( 1991 & september 1996 ) both times occurring in the right eye. During his first attack ( in Finland ) he was investigated for iritis ( Blood tests and X-ray to lower back) all tests were negative . He was then treated with topical steroids .
PMHx: Negative
Meds: Non No known allergy
FHx: Non-contributory
Pupils: Equal, reactive, No APD
Motility: Full OU
Applanation pressure: 10 OD, 16 OS
Slit lamp examination: See Figures 1-3
Fundus examination: Cup to disk ratio was 0.3 OD and O.6 OS. Macula and vessels were normal. No vitritis was present.
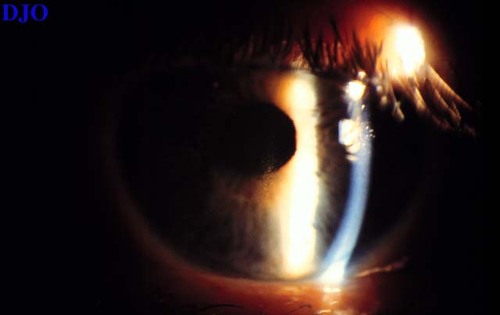
Figure 1a
There is deposition of particulate material on the corneal endothelium
There is deposition of particulate material on the corneal endothelium

Figure 1b
On higher magnification this appeared to be pigment. There was no cell or flare present.
On higher magnification this appeared to be pigment. There was no cell or flare present.

Figure 2
Iris transillumination is present when light is shined only through the pupil and the room lights are turned completely off.
Iris transillumination is present when light is shined only through the pupil and the room lights are turned completely off.
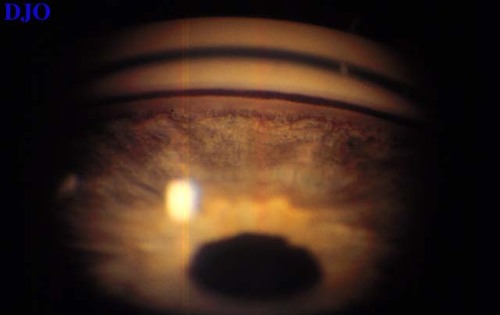
Figure 3
Gonioscopy revealed increased pigmentation of the angle OU (OS>OD)
Gonioscopy revealed increased pigmentation of the angle OU (OS>OD)
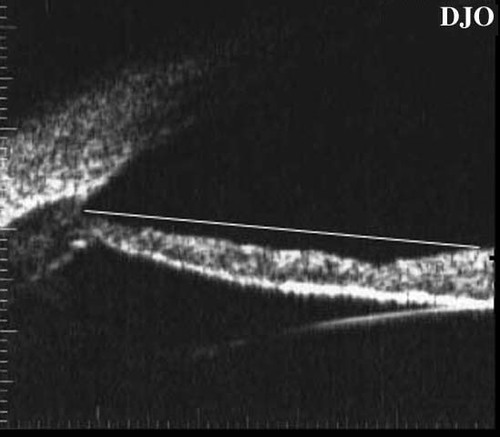
Figure 4
Ultrasound biomicroscopy demonstrates posterior bowing of the iris.
Ultrasound biomicroscopy demonstrates posterior bowing of the iris.
- Exfoliation syndrome
- Uveitis
- Ciliary ring melanoma
Pigmentary dispersion was first described by Von Hippel in1899 . Later Levinsohn suggested that glaucoma in this condition is related to pigment released FROM iris pigment epithelium. Many years later several investigators agreed or disagreed about the association between pigment and glaucoma . In the recent literature more evidence appeared supporting the association between pigment and glaucoma . Scheie & Cameron in 1981 studied a large number of patients confirmed the association .
Pigmentary dispersion syndrome ( PDS ) is a bilateral condition , although it can be asymmetric. It affects males more often with a peak at the fourth decade of life ( 35-45 ) . Over 80 % of patient are myopic and usually of mild to moderate myopia . It is a relatively common condition and often is overlooked. In the recent literature an autosomal dominant inheritance pattern was described in 4 families FROM Europe .The gene was mapped to 7q35-36 locus . The ocular findings in PDS is bilateral as described earlier. Krukenberg's spindle, a vertical deposition of pigment is due to aqueous convection currents in the anterior chamber. Endothelial deposits of pigment cells are not believed to interfere with endothelial function. The presence of pigment in the anterior chamber is often mistaken as anterior uveitis, our patient gave a history of treatment with topical steroids for presumed uveitis . Iris transillumination is characteristically in mid - periphery in contrast to pseudo-exfoliation which is at the pupil margin . Counting iris defect spokes can be helpful in following the progression of these patients . The most accepted theory for pigment release is posterior irido-zonular contact resulting in mechanical friction and release of pigment FROM posterior iris surface . This has been clearly shown pathologically.
What causes the iris to be posteriorly displaced and causes the contact ? The most accepted explanation is that during blinking, there is transient increase in anterior chamber pressure compared with posterior chamber (due secondary to reversed pupil block ) . The sagged iris becomes bows backwards resulting in irido-zonular contact. Pigment will then be deposited in the angle. Although the pigmentation is seen 360 degrees, it is best seen at the 12 O'clock angle. Occasionally a second line of pigment anterior to TM is seen ( Sampaolesi line ). Another site of pigment deposition is at the posterior lens capsule ( Scheie`s stripe ) . The degree of pigment in the angle poorly correlates with intraocular pressure . The condition was classified INTO 2 stages clinically & pathologically. Stage 1 ( reversible stage ) were the liberated pigment enters the intratrabecular spaces & being phagocytosed . At this stage intraocular pressure ( IOP ) is normal but may SHOW degree of fluctuation higher than normal physiological diurnal fluctuation . In addition there are some provocative factors that result in increase IOP ( due to transient trabecular decompensation ) , these factors include 10 % phenylephrine & exercise both result in increase pigment release . Stage 2 is the irreversible stage pathologically seen as trabecular sclerosis. At this stage aqueous suppressants play a small role in management . The prevalence of glaucoma & ocular hypertension in eyes with PDS is variable.The prevalence varied FROM 6 % ( 202 patients) by Evans to 25.6 % ( 407 patients ) by Scheie & Cameron .
Management of this condition can be challenging . Many people advocate close follow up of these patients with frequent assessments including visual fields especially because some of these patients may have tilted discs which is often difficult to follow. Once there is any suspicion about glaucoma treatment is recommended . Recently a prophylactic peripheral iridotomy has been shown by more than one GROUP of investigators to be effective . This has clearly been demonstrated by UBM were after PI iris position has changed as clearly demonstrated initially by Potash et al (Ophthalmology :101 # 2 , Feb 1994 ). Other treatment options are medical with aqueous suppressants. Pilocarpine is less commonly used because of its side effects in younger individuals. However, some people tolerate the slow release (Ocusert ) better than pilocarpine drops . It is important to note that the risk of retinal detachment in these patient is higher than the general population. Filtering surgery is an option in uncontrolled increased IOP . Greater percentage of eyes with PDS ( 23.5%) require filtering surgery when compared with eyes with primary open angle glaucoma ( 14.5%).