38 year old male complaining of "seeing spots" OS
Digital Journal of Ophthalmology 1997
Volume 3, Number 22
June 25, 1997
Volume 3, Number 22
June 25, 1997
Pupils: Equal, reactive, No APD
Motility: Full OU
Applanation pressure: 12 OD, 7 OS
Slit lamp examination: Normal OU except 1+ cell/flare OS
Fundus examination: See Figures 1a-1b
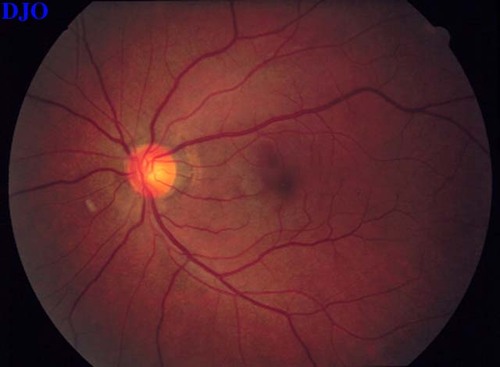
Figure 1a
Dilated fundus photograph OS
Dilated fundus photograph OS

Figure 1b
Close up OS
Close up OS
Surgical Approach for implanting ganciclovir implant:
1) Pars Plana incision inferotemporally
2) 0.5 ml of vitreous removed
3) Implant placed through wound and sutured to sclera
4) Wound closed and IOP restored
Follow-Up
- Received Ganciclovir intraocular implant
- Nasal periphery developed small retinal tear with localized subretinal fluid
- Retinal tear treated with cryotherapy with resolution of fluid
- Final visual acuity 20/30 OS
The diagnosis of CMV Retinitis in this HIV positive male with a low CD4 count was never in doubt. The question is how best to treat this patient.
Treatment options include:
- Induction with IV Ganciclovir
- Induction with IV Foscarnet
- Intraocular Ganciclovir pellet implant with or without oral Ganciclovir
Treatment Plan
The patient was treated with induction therapy using IV Ganciclovir for 2 weeks BID, followed by maintenance QD. On examination 2 months after treatment began, the patient noted HAVING photopsia for 1 week.
Vision: 20/40 OD, 20/20 OS
Pupils: Equal, reactive, No APD
Motility: Full OU
Applanation pressure: 14 OD, 10 OS
Slit lamp examination: Normal OU Deep/Quiet OU
Fundus examination: See Figures 2a-2b
Impression: Progression of CMV Retinitis OS
How would you treat this patient now?
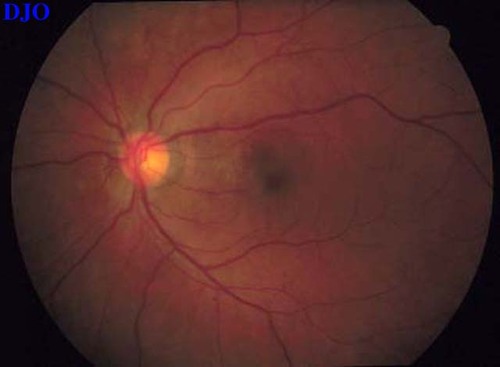
Figure 2a
Dilated fundus photograph OS
Dilated fundus photograph OS
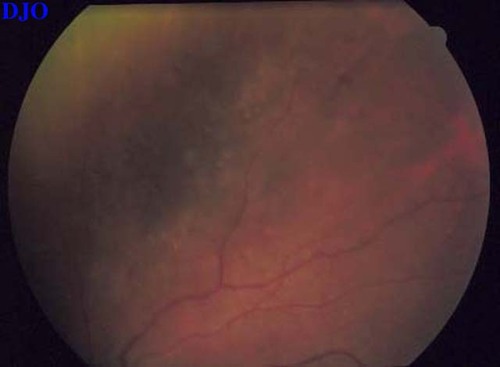
Figure 2b
Close up OS
Close up OS
Cytomegalovirus is the most frequent opportunistic ocular infection in AIDS patients, developing in 20-25% of patients. Ocular infection is felt to be due to reactivation of CMV already present in body, and generally occurs when the CD4 count falls below 100. Clinically, two types of retinitis are seen. The hemorrhagic type usually affects the posterior pole with a ?crumbled cheese and ketchup? appearance. The granular type is most often seen in the periphery with a yellow, granular appearance, often without hemorrhages. Both forms are associated with infection of the inner retina. CMV Retinitis is invariably progressive without treatment. Even with treatment, reactivation occurs by 1 year in 30-50% of patients. Furthermore, retinal detachment occurs in 15- 30% of treated patients.
CMV Therapy
Ganciclovir and foscarnet are both approved for the treatment of CMV retinitis. Ganciclovir is a synthetic nucleoside analogue, which prevents DNA elongation. Investigation with ganciclovir for CMV began 1984, and it was FDA approved in 1989. The induction dose is 5 mg/kg IV BID with a maintenance dose of 5 mg/kg IV QD. These must be adjusted in the face of severe neutropenia or renal failure. The major side effects of ganciclovir are neutropenia, anemia and thrombocytopenia. Foscarnet is a pyrophosphate analogue, which inhibits DNA polymerase. Investigation with foscarnet for CMV began 1987, and it was FDA approved in 1991. The induction dose is 60 mg/kg IV TID with a maintenance dose of 60 mg/kg IV BID or 90 mg/kg IV QD. Great concern must be taken as to correct dosing in the face of renal failure. The major side effects of foscarnet are nephrotoxicity, seizures, and metabolic disturbances.
Other Possible Treatment Modalities
1) Ganciclovir intravitreal injections
2) Foscarnet intravitreal injections
3) Ganciclovir intraocular implant
4) Ganciclovir orally
5) Cidofivir (Vistide)
How To Approach Recurrence
1) Reinduction with IV therapy (least favorable)
2) Combination IV therapy (Ganciclovir & Foscarnet)
3) Switch to intravitreal injections with Ganciclovir, Foscarnet, or both
4) Intraocular Ganciclovir Pellet
5) IV Cidofivir
Advantages of Ganciclovir Intraocular Implant
- Direct delivery of drug to site of infection
- Avoid systemic toxicity of drug
- Avoid daily drug administration
- Avoid risk of line sepsis
Potential Disadvantages
- No protection of fellow eye
- Extraocular CMV infection (mostly GI)
- Need for surgical procedure
Anand et al studied 30 eyes that received intraocular ganciclovir implants. 77% of patients had shown previous progression of CMV on IV ganciclovir. 90% of eyes showed initial stabilization and 47% maintained VA of 20/40 or better. 23% of patients developed systemic CMV. Adverse events included:
- Mild vitreous hemorrhage (11%)
- Astigmatism (11%)
- Corneal dellen (3%)
- Retinal detachment (11%)
Martin et al prospectively studied 39 untreated eyes that received intraocular ganciclovir implant that delivered drug at a rate of 1 mg/hr. The implant life span was approximately 8 months. The mean time to progression was 226 days in the treated GROUP compared with 15 days in deferred treatment group. The median survival was 295 days. 87% of treated eyes maintained VA of 20/25 or better. Retinal detachment developed in 18% of eyes, with a retinal tear without RD in 1 eye (2.6%). Biopsy-proven symptomatic visceral CMV developed in 31% of patients and CMV in fellow eye developed in 67% of patients with unilateral CMV.
Marx et al examined the efficacy of ganciclovir intraocular implants in recurrent CMV retinitis. 91 eyes of 70 patients received the implant with 76% of eyes achieving inactivity of CMV retinits after 1 month. 36% of eyes developed recurrent retinits, with a median time to recurrenc eof 7 months. The majority of the patients in the study continued on systemic anti-CMV therapy after receiving the implant. Final visual acuity remained the same in approxiamtely 50% of eyes. Retinal detachment was reported in 23% of patients at 6 months of follow-up. Other complications included vitreous hemorrhage, hyphema, and suprachoroidal placement of the device.
The Syntex study, a prospective, randomized clinical trial compared the efficacy of intravenous ganciclovir with the intraocular ganciclovir implant in previously untreated eyes with CMV retinitis. The implant GROUP was further randomized to receive either oral ganciclovir at a the dose of 1500 mg three times daily or placebo in ORDER to determine the benefit of oral ganciclovir as prophylaxis to protect the fellow eye and systemic CMV infection. The results of the Syntex study should be available later in 1996 and should further illuminate this rapidly developing area of ophthalmology.
2) Sanborn GE, Anand R, Torti RE et al. Sustained-release ganciclovir therapy for treatment of cytomegalovirus retinitis. Arch Ophthalmol. 1992;110:188-195.
3) Anand R, Nightingale SD, Fish RH, Smith TJ, Ashton P. Control of cytomegalovirus retinitis using sustained release of intraocular ganciclovir. Arch Ophthalmol 1993;1993:223-227.
4) Anand R, Font RL, Fish RH, Nightingale SD. Pathology of cytomegalovirus retinitis treated with sustained release intravitreal ganciclovir. Ophthalmology. 1993; 100:1032-1039.
5) Martin DF, Parks DJ, Mellow SD, et al. Treatment of cytomegalovirus retinitis with an intraocular sustained-release ganciclovir implant. Arch Ophthalmol. 1994:112:1531-1539
6) Marx JL, Kapusta MA, Patel SS, et al. Use of the ganciclovir implant in the treatment of recurrent cytomegalovirus retinitis. Arch Ophthalmol. 1996;114:814-820.