A 69 year old woman with a painful, red, right eye for two days
Digital Journal of Ophthalmology 1997
Volume 3, Number 19
May 28, 1997
Volume 3, Number 19
May 28, 1997
PMHx: None
PSHx: Appendectomy
Meds: None
SHx: Non contributory
FHx: None
Pupils: Equal, briskly reactive to light. No RAPD
Slit lamp examination: Normal OU
Extraocular Movements: Normal OU
Fundus examination: Normal OU
External: A firm, cystic mass was affixed to the lateral aspect of the orbital floor just posterior to the orbital rim. The posterior border of this lesion could not be appreciated clinically.

Figure 1
This is a photograph of the patient's right eye and orbit
This is a photograph of the patient's right eye and orbit
Pathology
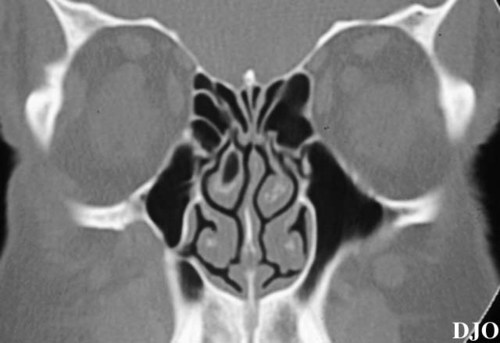
Figure 2
Figures 2-3. A non-contrast CT of the orbits (coronal images) was obtained. A lesion corresponding to the clinical mass was noted in the inferolateral aspect of the right orbit affixed to the orbital bone. The mass was only slightly more radio-dense than the surrounding orbital fatty tissues, and its margins were not clearly demarcated. There were several areas where the orbital bones overlying the maxillary sinus appeared to be eroded by this mass.
Figures 2-3. A non-contrast CT of the orbits (coronal images) was obtained. A lesion corresponding to the clinical mass was noted in the inferolateral aspect of the right orbit affixed to the orbital bone. The mass was only slightly more radio-dense than the surrounding orbital fatty tissues, and its margins were not clearly demarcated. There were several areas where the orbital bones overlying the maxillary sinus appeared to be eroded by this mass.

Figure 3
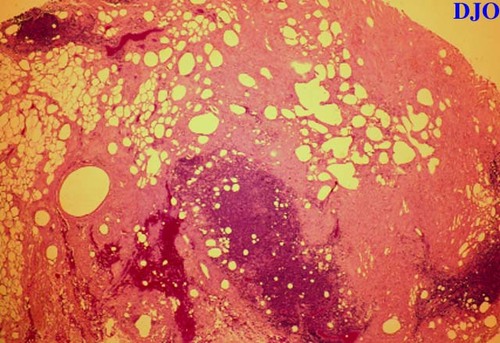
Figure 4
Figures 4-5. Pathology Specimens An orbitotomy with excisional biopsy was performed. Pathologic examination of frozen sections disclosed fibrosis and chronic granulomatous inflammation centered around foci of birefringent foreign material (Figure 4.). The birefringent material was noted to dissolve in processing and paraffin embedding suggesting a lipid composition (Figure 5.). These findings were consistent with a diagnosis of paraffinoma with foreign body inflammatory reaction.
Figures 4-5. Pathology Specimens An orbitotomy with excisional biopsy was performed. Pathologic examination of frozen sections disclosed fibrosis and chronic granulomatous inflammation centered around foci of birefringent foreign material (Figure 4.). The birefringent material was noted to dissolve in processing and paraffin embedding suggesting a lipid composition (Figure 5.). These findings were consistent with a diagnosis of paraffinoma with foreign body inflammatory reaction.
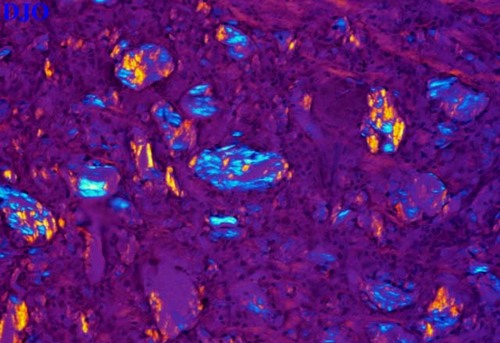
Figure 5
- Foreign body reaction
- Orbital pseudo tumor
- Neoplastic mass lesions
- Lymphoma
- Fibrous histiocytoma
- Maxillary sinus tumor (i.e. squamous cell carcinoma)
- Metastatic disease (i.e. prostate, lung)
- Chronic infectious process
The pathologic diagnosis of a paraffinoma was difficult to understand on the basis of the patient’s history up until this point. After thorough discussion, the patient added that he had sustained a wartime injury in Vietnam (29 years prior to his surgery). His description of the injury suggested that he had a right tripod fracture repaired by a Caldwell-Luc approach. After this surgery, he recalled HAVING several yards of Vaseline-impregnated gauze packing in his nasal sinuses. It is important to note that patients frequently omit historical information that they have simply forgotten or that they feel is irrelevant.
The pathologic DATA and the additional clinical DATA provided good evidence for a paraffinoma. Vaseline (similar to paraffin oil) is postulated to percolate through various tissue planes forming small collections of oil scattered within the tissues of the orbit. These collections subsequently incite a granulomatous response in the involved tissues.
One unique aspect of this case was the 29 year symptom-free interval between the surgery and the onset of orbital symptoms. In a recent series of 10 similar cases, Witschel and Geiger found that the interval between sinus procedures and orbital symptoms varied between several months and 4 years with recurrences as late as 15 years. Several possible scenarios can be postulated. Perhaps the Vaseline material was sequestered in the maxillary sinus until a recent event allowed the material to infiltrate the orbit, inciting a granulomatous response. Alternatively, the material may have been present within the orbit for many years before triggering an inflammatory response. It remains to be seen whether this procedure will alleviate his symptoms permanently.
2) Spencer WH. Persistent Orbital Paraffinoma. Presented at the Combined Meeting of the Hogan and Theobald Societies (1996)
3) Witschel H, Geiger K. Paraffin induced sclerosing lipogranuloma of eyelids and anterior orbit following endonasal sinus surgery. Br J Ophthalmol 78:61-65 (1994)