A 15-year-old-boy with an optic neuropathy
Digital Journal of Ophthalmology 2017
Volume 23, Number 4
December 5, 2017
DOI: 10.5693/djo.03.2015.06.001
Volume 23, Number 4
December 5, 2017
DOI: 10.5693/djo.03.2015.06.001
Download PDF

Figure 1
External photographs taken 7 days following the incident showing the temporal subconjunctival hemorrhage, eyelid ecchymosis, and mild proptosis in the left eye (A) and the entry site of the pellet in the left temple (B).
External photographs taken 7 days following the incident showing the temporal subconjunctival hemorrhage, eyelid ecchymosis, and mild proptosis in the left eye (A) and the entry site of the pellet in the left temple (B).
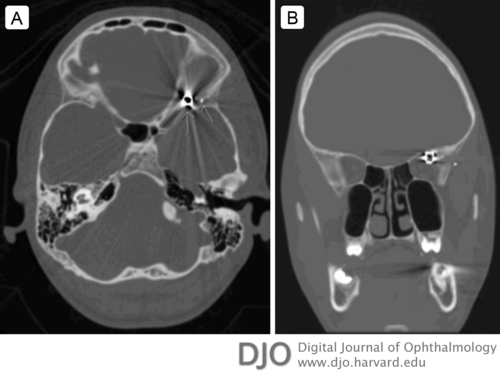
Figure 2
Computed tomography of the head. A, Axial scan showing the 4.5 mm metallic foreign body located in the apex of the left orbit; also visualized is a smaller shrapnel fragment lodged in the inner aspect of the left temporalis muscle. B, Coronal scan showing the path of the pellet through the left temporalis muscle and fractured lateral orbital wall, stopping short of and immediately adjacent to the optic nerve within the apex.
Computed tomography of the head. A, Axial scan showing the 4.5 mm metallic foreign body located in the apex of the left orbit; also visualized is a smaller shrapnel fragment lodged in the inner aspect of the left temporalis muscle. B, Coronal scan showing the path of the pellet through the left temporalis muscle and fractured lateral orbital wall, stopping short of and immediately adjacent to the optic nerve within the apex.
Postoperatively, the patient was admitted to the pediatric neuro-critical care unit. Repeat CT scan showed no evidence of acute intracranial hemorrhage or sulcal effacement. On postoperative day 1, there was complete resolution of the left afferent pupillary defect, and the patient’s visual acuity returned to 20/20 in the left eye. The patient was discharged on postoperative day 4 with resolution of eye pain and no restriction in his extraocular movements. He was followed closely for 3 months, with no further complications.
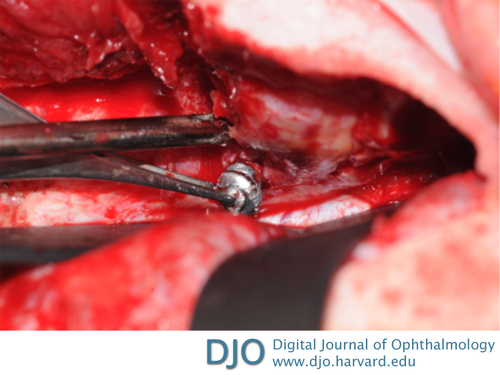
Figure 3
Intraoperative photograph showing the reflected left frontal lobe of the brain and demonstrating the extraction of the pellet lodged in the posterior apex of the left orbit, through the removed orbital roof and incised periorbita.
Intraoperative photograph showing the reflected left frontal lobe of the brain and demonstrating the extraction of the pellet lodged in the posterior apex of the left orbit, through the removed orbital roof and incised periorbita.
Most metallic foreign bodies are inert and should be managed conservatively if there are no other indications for surgery.(4) Copper, iron, and pure lead (that is, lead not mixed with antimony) are three metals that are not inert and require a more vigorous investigation, because they have been documented to cause both local and systemic complications.(4) On our patient’s presentation, we contacted the pellet manufacturer, who confirmed that the pellet used was 99.9% lead, which by itself might warrant removal if the foreign body is readily accessible. In many instances the composition of the metallic foreign body can never be determined, which often complicates the decision for surgical removal.
In our patient, several presenting factors determined the necessity for surgical removal. The decreased visual acuity in the left eye along with an afferent pupillary defect indicated a compressive optic neuropathy resulting from the location of the pellet in the apex in proximity to the optic nerve and resultant compressing edema in a tight compartment. Fortunately, the projectile did not directly injure the optic nerve. In the absence of any brain injury, there was no contraindication for steroids. The patient was started on oral prednisone 40 mg (1 mg/kg/day) in attempt to improve the orbital edema and decrease the optic nerve compression while awaiting surgical decompression and removal of the retained foreign body material.
A decision was made for a left transcranial orbitotomy with a cranio-orbital approach for removal of the foreign body. The posterior location of the pellet in the orbital apex eliminated an anterior orbitotomy approach. A lateral approach could have been used yet it would have required an osteotomy extending along the lateral orbital wall that was posteriorly fragmented. This would have required enlarging the bony incision of a classic lateral orbitotomy and removing the sphenoid wing to the superior orbital fissure, as described by Goldberg et al.(5) This approach would have eliminated the need for a craniotomy; however, it was possible that this might not have provided enough access and exposure to safely extract the pellet. A multidisciplinary team included our neurosurgery service who performed a left transcranial orbitotomy with a cranio-orbital approach and provided access for our oculoplastic surgery team. A cranio-orbital approach allowed for direct visualization of the superior orbital space, including the apex, and the pellet was easily removed without injuring vital structures. This approach also allowed for adequate exploration of the surrounding tissue for removal of smaller fragments within the orbit. In addition, the shrapnel lodged within the surgically reflected left temporalis muscle was removed.
2. Spoor TC. Penetrating orbital injuries. In: Spoor TC, Nest FA, eds. Management of Ocular, Orbital, and Adnexal Trauma. New York: Raven; 1988:271-92.
3. Orcutt JC. Orbital foreign bodies. In: Linberg JV, ed. Oculoplastic and Orbital Emergencies. Norwalk: Appleton & Lange; 1990:183-97.
4. Ho VH, Wilson, MW, Fleming, JC, Haik, BG. Retained intraorbital metallic foreign bodies. Ophthal Plast Reconstr Surg 20:232-6.
5. Goldberg RA, Shorr N, Arnold AC, Garcia GH. Deep transorbital approach to the apex and cavernous sinus. Ophthal Plast Reconstr Surg 1998;14:336-41.