39 year old Hispanic woman with a ten year history of gradual blurring of vision in both eyes
Digital Journal of Ophthalmology 1997
Volume 3, Number 16
April 2, 1997
Volume 3, Number 16
April 2, 1997
POHx: As above
PMHx: Non-contributory
Meds: None
SHx: Non contributory
FHx: None
Potential acuity meter: 20/50 OU
Pupils: Reactive OU, No relative afferent pupillary defect
External exam: Mild ptosis OU with fissure heights of 6 mm in each eye
Slit lamp examination: Scattered focal white superficial corneal stromal opacities more numerous centrally; subtle epithelial elevations associated with the focal opacities; diffuse stromal haze spans center to limbus; endothelial opacities are present. Corneal findings are bilateral and symmetric.
Fundus examination: Within normal limits OU
Management: The patient underwent penetrating keratoplasty OS.
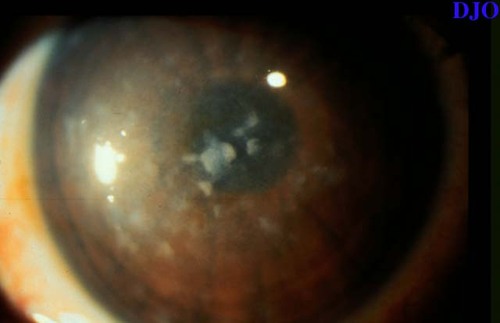
Figure 1
Anterior segment photograph of the patient's left eye. The patient's right eye had the same appearance.
Anterior segment photograph of the patient's left eye. The patient's right eye had the same appearance.

Figure 2
Appearance of the left eye post penetrating keratoplasty
Appearance of the left eye post penetrating keratoplasty
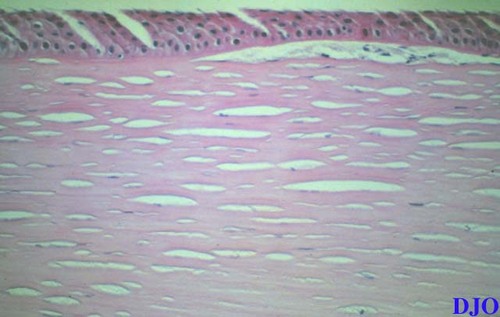
Figure 3
Figures 3-4. The left photograph shows the histopathology of the corneal button with Hematoxylin and Eosin stain. This demonstrates clear spaces surrounding the keratocytes and in the stroma. Alcian blue stain is positive for mucopolysaccharide material within the stroma.
Figures 3-4. The left photograph shows the histopathology of the corneal button with Hematoxylin and Eosin stain. This demonstrates clear spaces surrounding the keratocytes and in the stroma. Alcian blue stain is positive for mucopolysaccharide material within the stroma.
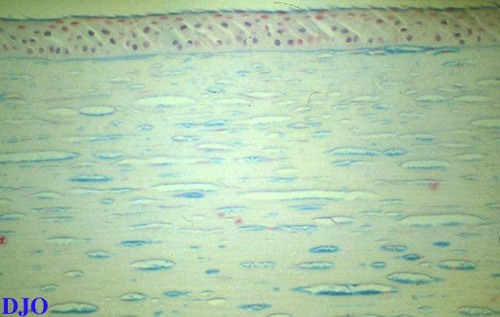
Figure 4
- Granular corneal dystrophy
Macular dystrophy is the least common of the 3 classic stromal dystrophies and the only one that has an autosomal recessive inheritance pattern (1). Macular dystrophy is a bilateral, symmetric disease that appears in the first decade of life and affects the central portion of the anterior layers of the stroma. Diffuse, grayish white spots with indistinct edges are seen. By the third decade, the diffuse stromal opacity with its ground glass appearance extends posteriorly to the endothelium and laterally to the limbus. Within it are small irregular, white patches that continue to expand, enlarge, and become more confluent. Late in the course of the disease, Descement's membrane becomes opacified and there are endothelial guttate changes. The epithelium remains smooth until the late stages of the disease, when the subepithelial opacities cause elevations and irregularities of the corneal surface. In the late stages, the vision is also reduced, and infrequently there are recurrent erosions and decreased corneal sensation.
There are two types of macular dystrophy distinguished by their biochemical characteristics. Type 1 is the more prevalent type. Antigenic keratan sulfate is missing FROM the cornea, serum, and cartilage due to a defect in the specific sulfotransferase involved in the sulfation of lactose-aminoglycans and abnormal unsulfated keratan-aminoglycan is produced. In type 2, dermatan sulfate chains are 40% shorter than normal and the synthesis of both keratan and dermatan sulfates are 30% below normal.
Histopathologically, the opacities are accumulations of glycosylaminoglycans (GAG) within the endoplasmic reticulum. They are thought to accumulate because of an inability to break down corneal keratan sulfate. The deposits stain with Alcian blue and colloidal iron.
The established treatment is penetrating keratoplasty. The disease can recur in the graft with the recurrence rate thought to be inversely proportional to the graft size (2). Excimer laser phototherapeutic keratectomy has been attempted, but post-treatment vision may still be clouded by residual diffuse stromal haze (3).
2) Akova YA, Kirkness CM, McCartney AC, Ficker LA, Rice NS, Steele AD. "Recurrent macular corneal dystrophy following penetrating keratoplasty." Eye 4:698 (1990)
3) Wu WCS, Stark W, Green WR, "Corneal wound healing after 193-nm excimer laser keratectomy." Arch Ophthalmol 109:1426 (1991)