19 year old man with a "corneal abrasion"
Digital Journal of Ophthalmology 1997
Volume 3, Number 15
March 18, 1997
Volume 3, Number 15
March 18, 1997
POHx: No history of contact lens use, no past ocular history
PMHx: Asthma, environmental allergies
Meds: Ventolin PRN, seldane
SHx: Non contributory
FHx: Father with pollen allergy
Pupils: Reactive OU, No relative afferent pupillary defect
External exam: Mild ptosis OU with fissure heights of 6 mm in each eye
Slit lamp examination: See Figures 1-5
Fundus examination: Within normal limits OU
Management: The patient was started on pred forte q2hrs OD, cromolyn qid OU, cyclogyl bid OD, ciloxan BID OD, bandage CL OD. Corneal cultures were taken and the patient was referred to an allergist.

Figure 1
Figures 1-2. In the right eye, there was 3+ conjunctival injection, a superior epithelial defect, microcystic edema, and superficial corneal haze. In the left eye, there was 1+ conjunctival injection
Figures 1-2. In the right eye, there was 3+ conjunctival injection, a superior epithelial defect, microcystic edema, and superficial corneal haze. In the left eye, there was 1+ conjunctival injection
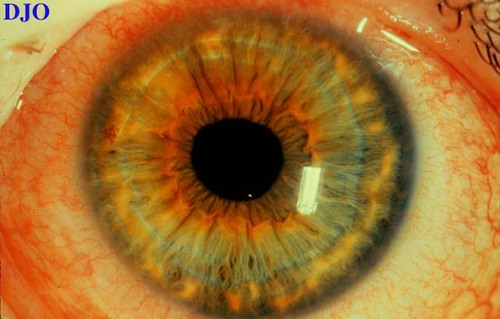
Figure 2

Figure 3
Figures 3-5. The epithelial defect on the right cornea was well dilineated with rose bengal stain. Lid eversion revealed large cobblestone pappilae OU which were covered in a tenacious mucous.
Figures 3-5. The epithelial defect on the right cornea was well dilineated with rose bengal stain. Lid eversion revealed large cobblestone pappilae OU which were covered in a tenacious mucous.
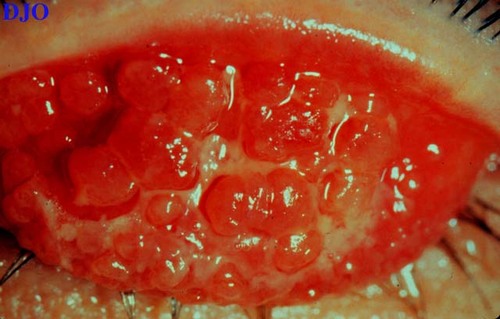
Figure 4

Figure 5
The patient returned to the cornea service several days after presentation. He was not tolerating the bandage contact lens and there had developed 15% thinning of the cornea. The superior tarsal papillae of the right upper lid were shaved in an attempt to decrease the mechanical irritation of the papillae and to reduce the amount of inflammatory mediators secreted by the superior tarsal papillae.
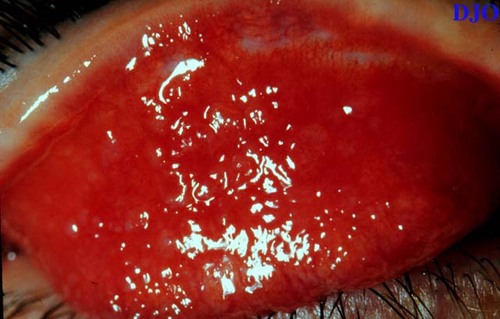
Figure 6
Appearance of the right superior tarsal conjunctiva after shaving of papillae
Appearance of the right superior tarsal conjunctiva after shaving of papillae
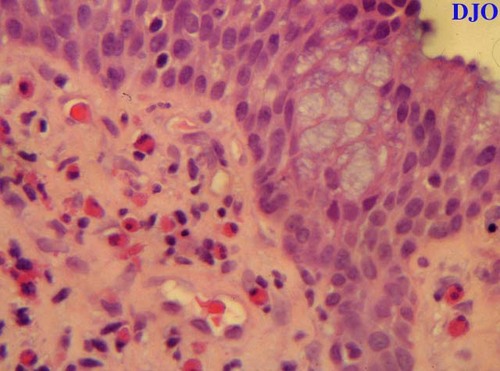
Figure 7
The shaved papillae were sent to pathology. The specimen demonstrated an abundant number of eosinophils (round cells with eccentric nuclei and bright pink cytoplasm).
The shaved papillae were sent to pathology. The specimen demonstrated an abundant number of eosinophils (round cells with eccentric nuclei and bright pink cytoplasm).
- Giant papillary conjunctivitis
- Vernal keratoconjunctivitis
- Trachoma
- Adult inclusion conjunctivitis
Clinical Course:
Four weeks after presenation the patient still had persistent epithelial staining with subepithelial haze. Cyclosporine 1% was started in addition to pred forte bid. Over the following 2 months the patient had resolution of his shield ulcer OD. The papillae of the right superior tarsus partly regrew. Six months after presentation the patient had complete resolution of his symptoms and was 20/20 OU.
Background:
The term vernal is derived FROM the Greek and means "occurring in the spring." Despite, this name, vernal keratoconjunctivitis (VKC) may occur during any season, although some patients do have seasonal exacerabtions. VKC has several interesting epidemiologic characteristics. Typically, it occurs more commonly in warm climates than cooler climates. It is often associated with a history of atopic disease such as asthma, allergic rhinitis, and eczema. There is also a male predominance with a male to female ratio of at least 2:1. Onset of the condition is frequently at puberty with remission occuring often by the late teens.
Clinical Features:
Patients usually present with symptoms of severe itching. Photophobia and pain may also be present if the corneal epithelium has been damaged. Because the symptoms of VKC may not differ significantly FROM those of seasonal allergic conjunctivitis, it is very important to evert the upper lids to rule out this entity.
The most characteristic examination finding of VKC are large raised conjunctival papillae on the upper tarsus. These "cobblestones" are almost never found on the lower tarsus. The upper lids may become so heavy FROM the presence of these cobblestones that a mechanical ptosis may result, as was the case in our patient. A tenacious stringy mucus is always present intertwined between the cobblestones. A well circumscribed sterile "shield" ulcer found on the superior or central aspect of the cornea is very typical of this condition.
There is a variant of VKC which preferentially affects the limbus. This form is more common in patients of African Descent and Asians. Findings in limbal VKC include Horner's Trantas dots which are elevated white superficial infiltrates that straddle the the limbus, with no intervening clear space. Gelatinous nodules representing enlarged limbal papillae are also found in this condition.
Pathophysiology:
It is believed that mast cells and eosinophils play critical roles in the pathogenesis of this allergic disease. Both mast cells and eosinophils are found in increased numbers in the conjunctiva of patients with VKC. The presence of 2 or more eosinophils per high power field in a biopsy of conjunctiva is essentially pathognomonic of VKC.
Treatment:
The first step in treating VKC, as well as all other allergic conditions of the eye, is to identify the allergen. Once the allergen is identified, the patient can then learn to eliminate or avoid the antigen. The aid of an allergist may be very helpful in this regard. Topical therapy may include brief courses of steroids (up to several weeks) to quiet the disease, followed by rapid tapering. Mast cell stabilizers including cromolyn and lodoxamide should be started while the patient is receiving steroids for acute flares since these agents require time for their clinical effects to occur. Once the acute situation is controlled some patients are able to be successfully treated with mast cell stabilizers alone. Other drugs that are being tried include cyclosporine and levocabastine. As was noted above, VKC often spontaneously remits after the late teens.
2) BenEzra, D. Pe'er J. Brodsky M. et al. Cyclosporine eyedrops for the treatment of severe vernal keratoconjunctivitis. Am J of Ophthalmol, 101:278 (1986)