7 year old girl with a left face turn and binocular diplopia
Digital Journal of Ophthalmology 1997
Volume 3, Number 13
February 18, 1997
Volume 3, Number 13
February 18, 1997
PMHx: None
Meds: None
SHx: Non contributory
FHx: None
Pupils: Equal, briskly reactive to light. No RAPD
External: 40 degree left face turn with chin up positioning.
Motility: 8 prism diopters of right hypotropia in primary gaze which increased to 12 prism diopters on left gaze and decreased to 3 prism diopters on right gaze. Limitation of elevation in adduction was noted with minimal to no elevation deficit in abduction. A 10 prism diopter exotropia was noted in upgaze only.
Stereo: 40 seconds of stereo with chin up
Cycloplegic refraction: +0.75 sphere ou
Slit lamp examination: Normal OU
Extraocular Movements: Normal OU
Fundus examination: Normal OU
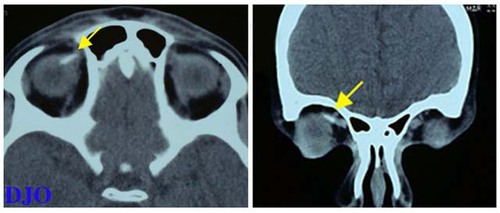
Figures 1a-1b
CT scan of head, without contrast, with attention to the orbits. Notable is the density located in the right superomedial orbit consistent with the previous superior oblique tendon expansion. Otherwise the imaging study was normal
CT scan of head, without contrast, with attention to the orbits. Notable is the density located in the right superomedial orbit consistent with the previous superior oblique tendon expansion. Otherwise the imaging study was normal
- Blowout fracture: Secondary to tissue entrapment or scarring. Restriction to elevation in abduction and adduction is equal or greater in the field of action of the superior rectus. Forced duction positive.
- Superior oblique overaction:. Forced duction with free passive elevation, "A" pattern exotropia, and inferior oblique function is normal by duction.
- Congenital fibrosis syndrome: Bilateral, congenital, multiple EOM involvement including elevation deficiency, limitation of abduction and adduction and ptosis.
- Monocular elevation defect (double elevator palsy): Unilateral, congenital, elevation deficiency equal in abduction and adduction.
- Adherence syndrome: Follows surgery on the inferior oblique muscle. Restriction to elevation is greatest in lateral gaze.
Forced duction testing of the right eye revealed restriction to elevation in adduction. The left eye was normal. Therefore, the diagnosis of Brown's syndrome OD was confirmed. Treatment consisted of a right superior oblique tendon expansion with 6.0 mm silicone #40 retinal device. There were no surgical complications.
The postoperative course was complicated by diplopia in primary position. Motility revealed 16 PD right hypertropia in primary position and 20 PD right hypertropia in downgaze. A 4 PD right hypotropia was present in upgaze. The diplopia in primary gaze was successfully treated with a 13 prism diopter prism BD OD divided equally. Visual acuity was 20/25 OD and 20/20 OS.
Ten months postoperatively, the patient presented to the Wills Eye Hospital Emergency Department after she noted the acute onset of binocular diplopia while wearing the corrective lenses . She denied a recent history of trauma or upper respiratory infection. There was no pain or tenderness. Examination of the extraocular motility is presented in Figure 2.
A right face turn of 10 degrees was also noted. Forced duction testing of the left eye revealed restriction of elevation in adduction. The diagnosis of a noninflammatory, atraumatic acquired left Brown's syndrome was made.
Medical evaluation including a complete physical examination, CBC, RF, and ANA was normal. A CT scan was performed.

Figure 2
Extraocular motility demonstrated by the diagnostic positions of gaze. Notable is the lack of elevation of the left eye when adducted.
Extraocular motility demonstrated by the diagnostic positions of gaze. Notable is the lack of elevation of the left eye when adducted.
Brown's syndrome is characterized clinically by the following: deficient elevation of the affected eye in adduction, improved elevation in the midline, and normal elevation in abduction. Superior oblique overaction, if present, should be minimal at most. Midline elevation produces divergence, manifesting as a V pattern exotropia. Finally, positive forced duction test of the affected eye demonstrating restricted passive elevation in adduction confirms the diagnosis.
Other clinical manifestations which may be seen include: downshoot of the affected eye in adduction, widened palpebral fissure on adduction, anomalous head posture, and primary position hypotropia.
Brown's syndrome is classified as congenital or acquired depending on the age of onset, and constant or intermittent depending on the clinical course.
Most cases of congenital and constant Brown's syndrome are thought to be caused by developmental anomalies of the superior oblique tendon and/or trochlea apparatus. Most cases of acquired Brown's syndrome are idiopathic. However, Brown's syndrome may also develop secondary to inflammatory conditions such as juvenile rheumatoid arthritis, trauma to the superomedial orbit, mass lesions involving the superomedial orbit, and postoperatively following surgery on the superior oblique tendon, orbit, retina, or sinus.
The indications for treatment of Brown's syndrome are abnormal head position and significant hypotropia in primary position. However, most acquired cases should be observed for approximately one year since spontaneous improvement has been reported.
Treatment options include observation alone, injection of steroids near the trochlea in inflammatory conditions, superior oblique tenotomy, superior oblique tenectomy, simultaneous superior oblique tenotomy and inferior oblique muscle recession, and superior oblique tendon silicone expander.
Complications of treatment include signs and symptoms of a superior oblique muscle palsy and improved but persistent Brown's syndrome.
Key Points:
- The diagnosis of Brown's syndrome can be made when the classic motility defect is seen. The diagnosis is confirmed with positive forced duction testing in the affected eye.
- Acquired Brown's syndrome may be secondary to various inflammatory, neoplastic and post-traumatic conditions. Imaging studies and serologic testing are useful in the evaluation of underlying conditions.
- The most common management for all types of Brown's syndrome is observation. Acquired and intermittent cases have a higher rate of spontaneous regression than congenital and constant cases.
- The main indications for surgery in Brown's syndrome are primary position hypotropia and/or an anomalous head posture.