36 year old man with redness, discharge and blurred vision in the left eye
Digital Journal of Ophthalmology 1997
Volume 3, Number 11
January 21, 1997
Volume 3, Number 11
January 21, 1997
PMHx: Diabetes
Meds: Insulin
SHx: Drug and alcohol abuse
FHx: None
Pupils: 3mm OD, 4mm OS; sluggish OU without RAPD
External: Normal OU
Extraocular Movements: Normal OU
Corneal Sensation:
Slit lamp examination: OD diffuse punctate epithelial keratitis
Corneal Sensation: noted to be diminished bilaterally, prior to instillation of fluorocaine
Visual Fields: Full to confrontation
Fundus: Nonproliferative diabetic retinopathy
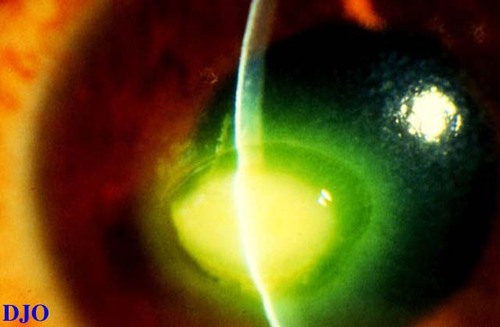
Figure 1
Cornea OS there is a round epithelial defect present with heaped up edges and dense infiltrate centrally
Cornea OS there is a round epithelial defect present with heaped up edges and dense infiltrate centrally
The ulcer was re-cultured, this time making an explicit effort to get deeper material FROM within the ulcer. Vancomycin was substituted for the cefazolin every 2 hours around the clock. After six days of this therapy, the patient's vision was finger counting at 2 feet, the ulcer was essentially unchanged in size, and the epithelial defect had enlarged. In addition, there was a hypopyon filling <5% of the anterior chamber.
A corneal biopsy was performed (see Figure 2).
As the ulcer was presumed to be sterile, a lateral tarsorraphy was performed on the left eye. Vigorous lubrication with bacitracin ointment and artificial tears was instituted. The antibiotics were discontinued. To date, the patient remains with significant corneal ulceration and, in fact, has developed similar corneal ulceration in the right eye as well, despite aggressive efforts and a tarsorrhaphy on that eye.
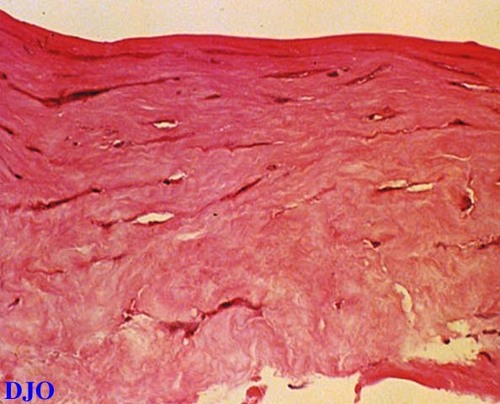
Figure 2
The pathology report on the tissue revealed no organisms and few white blood cells.
The pathology report on the tissue revealed no organisms and few white blood cells.
- Fungal corneal ulcer
- Parasitic corneal ulcer
- Sterile neurotrophic corneal ulcer
This patient presented with a corneal ulcer which was found on culture testing to be sterile. In combination with diminished sensation of the corneas, the diagnosis was neurotrophic corneal ulceration. The patient repeatedly denied any surreptitious use of proparacaine or other topical commercial anesthetics. He did admit to frequent crack cocaine smoking up to the day of admission to the rehabilitation facility. This history in combination with the negative culture results on two separate occasions as well as a negative corneal biopsy effectively rule out infectious corneal ulceration. We believe this patient suffered FROM a neurotrophic keratopathy related to what has been termed crack keratopathy to describe a spectrum of corneal disease resulting directly FROM the toxic effect of crack cocaine on the cornea.
In their paper describing this syndrome, Sachs, Zagelbaum, and Hersh describe 14 patients with a spectrum of corneal diseases ranging FROM superficial punctate keratopathy (SPK) to epithelial defects to frank corneal ulceration resulting directly FROM crack smoking. In their study, 10 patients had corneal ulcers, and of 7 patients with unilateral ulcers, 6 had diffuse SPK in the other eye as did our patient. Nine of 13 ulcers were culture positive, and 7 of those grew either Staph or Strep. One culture grew Candida albicans, and another grew both H. Flu and Streptococci viridans. Five of 10 patients tested had decreased corneal sensitivity, as did our patient.
Sachs, Zagelbaum, and Hersh postulate five different mechanisms of damage FROM crack: a directly toxic effect of smoke, exposure due to decreased sensation, neurotrophic effects resulting FROM damage to corneal nerves, mild alkali burn, and mechanical trauma occurring after rubbing the irritated eyes.
Our patient fits the above description of crack keratopathy in that he is a young man without other known risk factors that predispose to corneal ulceration. We have since seen two other patients with similar histories of crack abuse presenting with keratopathy. This entity appears to be a fairly common cause of neurotrophic ulceration in young patients, and should be considered in the appropriate clinical setting.
Key Points:
- When a patient presents with a corneal ulcer that has the classic appearance of an oval, smooth edged, inferior paracentral infiltrate with an overlying epithelial defect with rolled edges, the diagnosis of neurotrophic keratopathy must be strongly suspected.
- An assessment of corneal sensation is crucial in the evaluation of a patient with an unusual corneal ulcer or when the pain is not proportional to the clinical findings.
- Since a sterile corneal ulcer is a diagnosis of exclusion, it is incumbent upon the ophthalmologist to prove this by vigorous culture and even biopsy if necessary.
- A conjunctival swab has little diagnostic utility in the management of a patient with a corneal ulcer.
- A corneal ulcer arising in a young patient who is not a contact lens wearer and who has had no trauma is distinctly unusual and should prompt one to consider crack keratopathy in the differential diagnosis.
2) Strominger M, Sachs R, Hersh P. Microbial keratitis with crack cocaine. Arch Ophthalmol 108:672. (1990)
3) Zagelbaum B, Tannenbaum M, Hersh P. Candida albicans corneal ulcer associated with crack cocaine. Am J Ophthalmol 111:248-49.(1991)