44 year old man with 2 months of painless progressive visual loss OD
Digital Journal of Ophthalmology 1997
Volume 3, Number 10
January 7, 1997
Volume 3, Number 10
January 7, 1997
PMHx: None
Meds: None
SHx: Non contributory
FHx: None
Pupils: Equal, briskly reactive to light. A trace relative afferent pupillary defect was present in the right eye.
External: Normal OU
Slit lamp examination: Normal OU
Extraocular Movements: Normal OU
Fundus examination: significant only for moderate optic nerve pallor in the right eye.
Visual Fields: See Figures 1-2
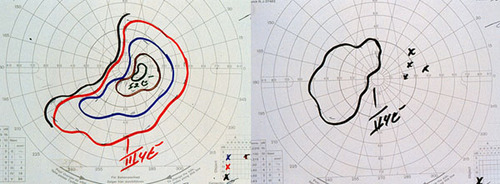
Figures 1-2
Figures 1-2. Goldmann visual field testing revealing a nasal island of field in the right eye, and a sloping superotemporal defect in the left eye.
Figures 1-2. Goldmann visual field testing revealing a nasal island of field in the right eye, and a sloping superotemporal defect in the left eye.
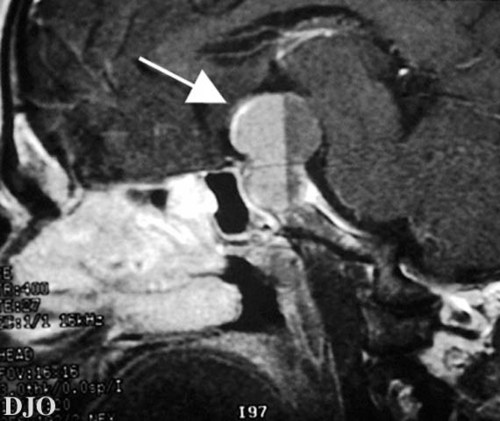
Figure 3
MRI of the brain with attention to the sella and suprasellar regions.
MRI of the brain with attention to the sella and suprasellar regions.
- Craniopharyngioma
- Meningioma
- Aneurysm
- Teratoma
Although the term pituitary apoplexy was originally used to describe a spontaneous infarction of nontumerous pituitary glands, current usage refers to infarction and necrosis of the pituitary gland which occurs in association with degeneration of an associated pituitary tumor.
Classically, pituitary apoplexy results when an acute hemorrhage INTO a pituitary adenoma produces an infarction of the gland and damage to adjacent structures such as the optic nerves and chiasm, ocular motor nerves, and hypothalamus. Subarachnoid hemorrhage, with signs of meningeal irritation and a progressive decrease in the level of consciousness, may also occur.
The diagnosis of pituitary apoplexy is suggested by the clinical findings and confirmed by neuroimaging studies. Both CT scanning and MRI are able to demonstrate a pituitary adenoma. Hemorrhage INTO the tumor may or may not be seen. In this case, a fluid-fluid level could suggest that hemorrhage had occurred.
The treatment of pituitary apoplexy consists of immediate treatment with high-dose intravenous corticosteroids. Careful attention should be paid to electrolyte levels. Urgent surgical removal of the tumor and/or hematoma should be considered in those cases with severe visual or mental impairment or progressive deterioration.
Most patients with pituitary apoplexy who are treated early with decompression surgery have reasonably good outcomes. Operative surgical mortality and morbidity are low, and it is not uncommon to regain significant amounts of visual function.
Key Points:
Although the left optic nerve appeared normal on exam, the process was thought to be bilateral because the afferent pupillary defect OD was not proportional to the amount of vision loss and optic nerve pallor.
Pituitary tumors which cause a chiasmal syndrome are large lesions and should be evaluated relatively urgently. This patient was seen by his general ophthalmologist only two weeks prior to this life-threatening episode.
Untreated pituitary apoplexy carries a high mortality rate. Hypopituitarism with secondary adrenal insufficiency results in severe electrolyte disturbances and hypotension if exogenous corticosteroids are not administered.
It is possible for patients to regain a significant amount of vision following surgical decompression of the optic nerves and chiasm.