39 year old Hispanic man who presents with decreased vision OS for one year
Digital Journal of Ophthalmology 1996
Volume 2, Number 10
December 24, 1996
Volume 2, Number 10
December 24, 1996
PMHx: Unknown
Meds: Rifampin 600 mg po qd and minocycline 50 mg po qd.
SHx: Non contributory
Pupils: No APD
External: leonine facies
Slit Lamp Exam:
- Lids: Absence of lashes OU. Loss of the tarsal plate more marked in the upper lids than in the lower ones OU; lid margins thickened OU
- Conjunctiva: Grade one plus follicles OU
- Sclera: quiet OU
- Cornea: punctate epithelial opacities superiorly OU with pannus formation.; prominent anterior stromal opacities; decreased corneal sensation in all quadrants.
- Anterior chamber: deep and quiet OU
Tonometry: Normal OU
Schirmer's Test: Normal OU
Fundus examination: The disc, macula, and vessels OU were within normal limits.
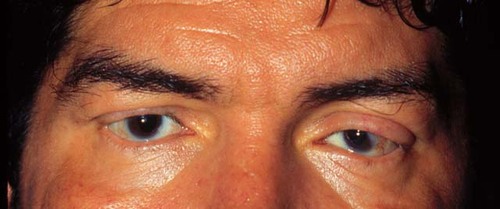
Figure 1
This is a racoon view of the patient's eyes. Please note the loss of eyelashes.
This is a racoon view of the patient's eyes. Please note the loss of eyelashes.

Figure 2
Figures 2-3. These are low and high power views of the patient's anterior segments. There are small discrete lesions on the surface of the iris, which are pointed out by the black arrows.
Figures 2-3. These are low and high power views of the patient's anterior segments. There are small discrete lesions on the surface of the iris, which are pointed out by the black arrows.
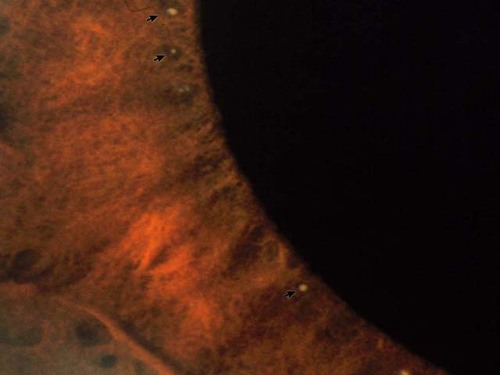
Figure 3
- Tuberculosis
- Cutaneous mycosis or lymphoma
- Neurofibromatosis
- Sarcoidosis
- Hansen's disease (leprosy)
This patient has ocular manifestations of lepromatous leprosy: loss of tarsal plates, thickened eyelids, madarosis of lashes and brows, iris pearls, corneal hypesthesia, and punctate keratitis. This diagnosis was confirmed by biopsy of a plaquelike lesion FROM his right dorsal forearm, which showed many acid-fast bacilli and foam cells. Diagnosis of lepromatous leprosy is best made by slit-skin biopsy, but a nerve biopsy may also be diagnostic.
Hansen's disease is a chronic granulomatous disease caused by Mycobacterium leprae. It affects 10 to 12 million people worldwide, about 15% of whom are blind FROM sequelae of the disease. However, there are only approximately 6,000 patients with leprosy in the United States. In this country, up to 350 new cases have been reported each year for the past 20 years. Ninety percent of these people have emigrated from, or traveled in, endemic areas abroad, which include Latin America, Asia, and Africa. Endemic areas within the United States are limited to Texas, Hawaii, Louisiana, and California.
There are two major types of leprosy, tuberculoid and lepromatous, and three subtypes in between--borderline tuberculoid, borderline lepromatous, and indeterminant type. The three subtypes in the middle of the spectrum have characteristics of both extremes. At the tuberculoid (paucibacillary) end of the spectrum, there is a strong cell-mediated immune response to the bacillus, characterized by granuloma formation and a relatively benign clinical presentation. Few bacilli are seen in biopsies. Ophthalmic manifestations tend to be limited to external ocular problems, such as lagophthalmos, superficial keratopathy, and corneal hypesthesia.
The lepromatous extreme is characterized by lack of cell-mediated immunity to the organism. Many bacilli are seen on histopathology, and hence the other name for this disease type is "multibacillary." Lepromatous leprosy is marked by a progressive, malignant course, and there are both extraocular and intraocular features. The causes of potential visual impairment in Hansen's disease include lagophthalmos, corneal hypesthesia, uveitis, and cataracts. Iridocyclitis is the most frequent cause of blindness in these patients. Punctate keratitis, corneal nerve beading, and iris pearls are more commonly seen in the lepromatous type than in the tuberculoid type; all three are pathognomonic for Hansen's disease. Iris pearls contain many bacilli, and with time, iris atrophy may occur. The choroid and retina are rarely affected, except perhaps through spread FROM the ciliary body to the choroid.
The differential diagnosis of Hansen's disease includes histiocytosis X, nummular eczema, lupus erythematosus, syphilis, unexplained facial nerve palsies, pityriasis rosea, erysipelas, tuberculosis, cutaneous mycosis, cutaneous lymphoma, neurofibromatosis, and sarcoidosis. There is no specific serologic test for Hansen's disease. Moreover, many patients are hyperglobulinemic and will have autoantibodies directed against cellular and nuclear antigens. They may also have false positive serologic tests for syphilis, as did this patient.
The treatment regimen not only depends on the disease type, but also varies amongst Hansen's disease specialists. The World Health Organization's guidelines on lepromatous leprosy consists of dapsone, clofazimine, and rifampin for 2 years. Other groups have suggested that long-term prophylaxis with dapsone after effective inital therapy may not be necessary. Yet others have recommended life-long treatment for lepromatous leprosy because of patients who were treated and yet have persistent positive biopies. Newer drugs include ofloxacin, clarithromycin, and minocycline. In treating borderline cases, cell-mediated immunity may be enhanced, causing an increased inflammatory response that may be even more detrimental than the disease itself. In such instances, steroids may be useful. Cytokine therapy is under investigation.
Treating the underlying disease type is necessary for addressing ocular complications. Complications that lead to loss of vision can be avoided or treated with relatively simple therapeutic measures. Lid plastic REPAIR and lubrication may be necessary for exposure keratopathy and trichiasis. Steroids (both topical and systemic) may be used in cases of acute iridocyclitis. Standard surgical treatment and intraocular lens implantation are appropriate for cataracts.
In conclusion, the eye is only one of many organ systems affected by Hansen's disease. It is important to treat the underlying disorder before one addresses the ocular manifestations. Simple measures can remedy many of the latter problems. Patients should have a thorough baseline ophthalmic examination combined with a program of regular follow-up.
2) Gelber RH Hansen's disease. Western Journal of Medicine. 1993; 158(6): 583-590.
3) Kaplan G. Recent advances in cytokine therapy in leprosy. Journal of Infectious Diseases. 1993; 167(1) Supplement 18-22.
4) Mannis MJ, Macsai MS, Huntley AC. Eye and Skin Diseases. Lippincott-Raven Publishers, Philadelphia, 1996.
5) Ostler H.B. Diseases of the External Eye and Adnexa. Williams & Wilkins, Baltimore, 1993:
6) Waddell KM Is leprosy blindness avoidable? The effect of disease type, duration, and treatment on eye damage FROM leprosy in Uganda. British Journal of Ophthalmology. 1995; 79(3): 250-6.
7) Walthen PI Hansen's disease. Southern Medical Journal. 1996; 89(7): 647-652.
8) Leprosy. Report of a meeting of physicians and scientists at the All India Institute of Medical Sciences, New Delhi. Lancet. 1995; 345(8951): 697-703.