60 year old man with ulcerated lesions of the right eyelid
Digital Journal of Ophthalmology 1996
Volume 2, Number 8
November 27, 1996
Volume 2, Number 8
November 27, 1996
PMHx: Chronic cough
Meds: None
SHx: Heavy smoker for several years. He was a rural worker since youth FROM the northeast of Argentina.
FHx: Unknown
Pupils: OD not well visualized, OS no APD
External: See Figure 1
Slit lamp examination: Epithelial and anterior stromal opacities.
Fundus examination: OD view precluded due to corneal opacity. Normal fundus OS. Normal posterior segment findings on ultrasonographic examination of the right eye.

Figure 1
Ulcerated lesions with necrosis and purulent exudation FROM the superior and inferior eyelids OD.
Ulcerated lesions with necrosis and purulent exudation FROM the superior and inferior eyelids OD.
Pathology
A biopsy of the right eyelid showed an ulcerated skin lesion with pseudoepitheliomatous epidermal hyperplasia. The tissue was infiltrated by a mixture of suppurative and granulomatous inflammation with multinucleated giant cells containing round structures. Grocott stain revealed the presence of intracellular and extracellular budding round yeasts, some of them with a ship's-wheel configuration consistent with Paracoccidioides brasiliensis.
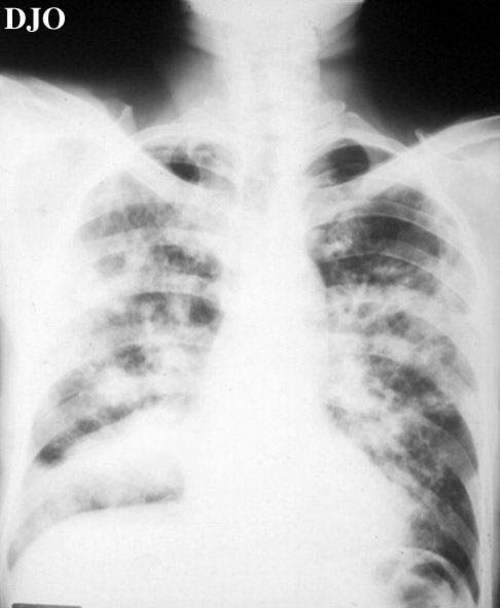
Figure 2
A chest radiograph showed multiple bilateral nodular lesions of the lung with collapse of the inferior right lobe. Computed tomography revealed a cavitated lesion with an air-fluid level.
A chest radiograph showed multiple bilateral nodular lesions of the lung with collapse of the inferior right lobe. Computed tomography revealed a cavitated lesion with an air-fluid level.
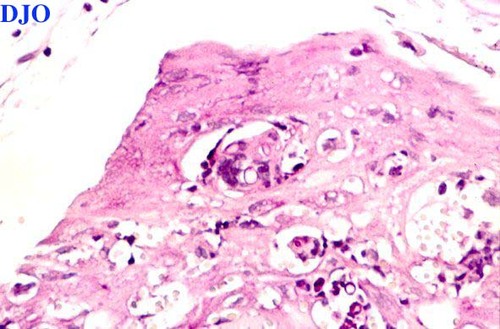
Figure 3
Figures 3-4. Epithelial hyperplasia with epithelioid and multinucleated giant cells containing round structures (PAS, X125). Groccott stain disclosing multiple budding yeast (X250)
Figures 3-4. Epithelial hyperplasia with epithelioid and multinucleated giant cells containing round structures (PAS, X125). Groccott stain disclosing multiple budding yeast (X250)
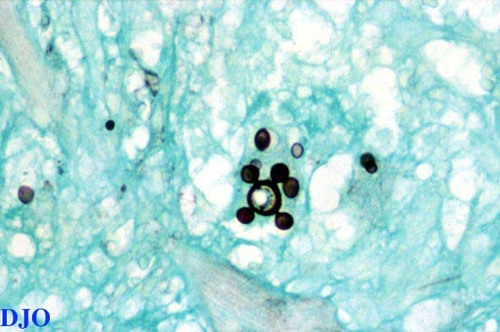
Figure 4
- Basal cell carcinoma
- Squamous cell carcinoma
- Leprosy
- Fungal infection
- Leishmaniasis
- Cutaneous lymphoma
Culture of the patient's sputum and bronchoalveolar washings grew Paracoccidioides brasiliensis. Cultures for mycobacteria gave negative results. The patient was started on oral Itraconazole 100 mg/day.
Paracoccidioidomycosis (Lutz-Splendore-Almeida's disease) is a granulomatous diseases caused by the dimorphic fungus Paracoccidioides brasiliensis. The infection is endemic in tropical and subtropical regions of South America, and may be seen in Central America, Mexico, and Africa. Occasional cases have been observed in the United States in patients traveling FROM countries where this mycosis is endemic. Male rural workers FROM 30 to 60 years of age constitute the population at risk. Paracoccidioides is most frequently acquired by inhalation of the organism. The primary lung infection may be asymptomatic and then disseminate to involve mucous membranes, lymph nodes, and other organs. The mucosal lesions are ulcerative with a serpiginous active border and a crusted surface. Microscopic examination is important for the diagnosis of paracoccidioidomycosis. Characteristic findings include large, round or oval, multiple budding yeast cells, 5 to 20 µm in diameter, that occasionally may resemble a ship's wheel. Nonbudding cells may resemble Blastomyces dermatitidis, Histoplasma and Coccidioides. Carcinomas have been associated with scarring after infection. Progressive chronic forms are treated with itraconazole for long periods.
2) Binford CH, Connor DH (eds): Pathology of Tropical and Extraordinary Diseases. Vol 2. Washington DC: Armed Forces Institute of Pathology; 567 (1976).
3) Rubinstein P, Negroni R (eds): Micosis broncopulmonares del niöo y el adulto. Buenos Aires: Editorial Betta, 2nd Edition, 183-5 (1981).
4) Kamegasawa A, Bet de Moraes Silva MR, Franco M, Heimbeck FJ. Paracoccidioides ocular: revisao. Arq Bras Oftalmol 51:183-5 (1988).
5) Slack JW, Hyndiuk RA, Harris GJ, Simons KB. Blastomycosis of the eyelid and conjunctiva. Ophthalmic Plastic and Reconstructive Surgery 8:143-9 (1992).