38 year old man who was hit in the left eye with a pool cue
Digital Journal of Ophthalmology 1996
Volume 2, Number 7
November 10, 1996
Volume 2, Number 7
November 10, 1996
PMHx: Depression
Meds: Zoloft
Allergies: no known drug allergies SHx: Non contributory
FHx: Non contributory
Pupils: OD 4 --> 2, OS irregularly shaped pupil, positive left APD
Motility: Full OD, motility limited OS to about 70% in all fields of gaze
External: See Figure 1
Slit lamp examination:
- OD within normal limits
- OS examination was as follows:
- Lids and lashes: ecchymosis
- Conjunctiva: chemosis
- Cornea: 2 x 2 medial epithelial defect
- Anterior chamber: +2 cells and flare, pathologically deep
- Iris: bowed posteriorly
- Lens: pushed slightly posterior with fibrin on anterior capsule
Tonometry: 12 OD, 13 OS
Fundus examination:
- OD within normal limits
- OS showed vitreous hemorrhage with a poor view. There was no obvious foreign body.

Figure 1
External photographs of the patient showing marked echymosis OS
External photographs of the patient showing marked echymosis OS
Figure 2
External photograph showing 360 degrees of bullous subconjunctival hemorrhage
External photograph showing 360 degrees of bullous subconjunctival hemorrhage

Figure 3
Demonstrates a superior orbital fracture on the left with fragments of bone extending toward the frontal lobe. There was no evidence of an optic canal fracture.
Demonstrates a superior orbital fracture on the left with fragments of bone extending toward the frontal lobe. There was no evidence of an optic canal fracture.
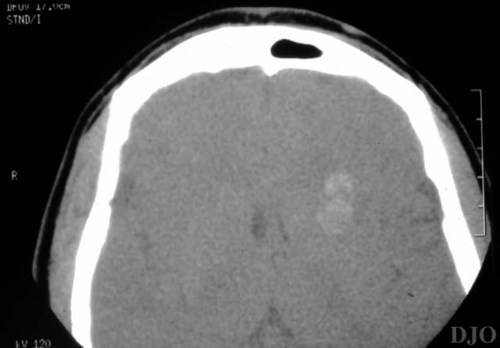
Figure 4
Illustrates the presence of hemorrhage present in the left frontal lobe.
Illustrates the presence of hemorrhage present in the left frontal lobe.
- Orbital edema and hemorrhage without a fracture
- Ruptured globe
- Intraocular foreign body
- Retinal detachment
- CNS involvement
- Traumatic optic neuropathy
Clinical Course:
The patient was admitted to the Massachusetts General Hospital (MGH) Neurosurgical service and placed on dilantin (for seizure prophylaxis) and IV antibiotics (nafcillin, ceftriaxone, and flagyl). Neurosurgery placed a bolt to monitor the patient's intracranial pressure (figure 5). Surgical exploration of the globe was done due to poor vision and possible globe rupture. A superior scleral rupture was found with extensive uveal prolapse (figure 6). The rupture extended 13 mm circumferentially in the superotemporal region, extending underneath the superior rectus muscle. The prolapsed uvea was repositioned and the scleral rupture was repaired.
The patient was given 5 days of neurosurgical observation for intracranial hemorrhage and IV antibiotics for the frontal sinus fracture and ruptured globe. Vitreoretinal consultation was arranged. The patient was then discharged on a topical ophthalmic regimen including antibiotics, steroid, and cycloplegia. By one week post-operatively, the patient’s vision OS was light perception. Ultrasound (US) was performed at this time. (Figure 7.)
After considering the risks and benefits, the patient declined vitreoretinal surgery.
Superior Orbital Fractures:
Isolated superior orbital fractures are rare. Orbital roof fractures usually occur in the setting of penetrating trauma or multiple facial fractures. Fractures of the orbital roof are much less common than those involving the floor. In a series of 457 patients with facial fractures, 5 patients had displaced orbital roof fractures (Sullivan, 1991). The orbital plate of the frontal bone is thin and easily fractured, especially in the region of the superior orbital fissure and the optic foramen.
The presumptive mechanism of injury to the orbital plate is usually backward transmission of forces FROM a blow to the superior orbital rim. Such force is frequently associated with head injury or frontal sinus fracture. The fractured roof fragments may be displaced upward or downward.
Early recognition of these fractures is important. The diagnosis of ocular injury may be obscured by more severe facial and cranial injuries which demand primary treatment. If treatment of orbital roof fracture is delayed beyond a few weeks, surgical REPAIR is more difficult due to fibrous scarring. Untreated large or comminuted roof fractures may result in late enophthalmos or motility dysfunction.
A variety of ophthalmic and neurologic injuries may be seen in the setting of an orbital roof fracture. Orbital edema, hematoma of the superior rectus or superior oblique muscles, and orbital hemorrhage, are usually self-limited. Impingement of the superior rectus muscle, or trochlear displacement causing impairment of superior oblique muscle generally require surgical repair. Injury of the 3rd, 4th, or 6th nerves at the superior orbital fissure can result in ophthalmoplegia. Ptosis is also common. Optic nerve contusion, nerve sheath hemorrhage, or nerve compression within the optic canal may result in visual loss. In some of these cases, optic nerve sheath decompression or orbital decompression may successfully return visual function.
Trauma to the forehead causing orbital roof fractures may also result in a subfrontal epidural hemorrhage. Other intracranial complications include cerebrospinal fluid leak, dural fistula and intracranial air. Prophylactic treatment with antibiotics to prevent meningitis is controversial. A delay in the onset of CSF leak, after the traumatic insult, increases the incidence of meningitis FROM 10% to 50%. Unilateral rhinorrhea usually indicates the side of the dural tear, but is not always reliable. Eighty percent of CSF leaks will spontaneously close, usually within 14 days.
Non-displaced fractures of the roof can usually be followed closely. Comminuted fractures, extensive roof fractures, and fractures with entrapment of orbital tissues generally require surgical treatment. Common surgical approaches to the orbital roof include the upper eyelid crease incision and the coronal flap. Major reconstructive efforts sometimes require a neurosurgical approach FROM the anterior cranial fossa. An interdisciplinary approach involving ophthalmologist, and neurosurgeon, or craniofacial surgeon is sometimes helpful. Because of the proximity to the central nervous system, the possibility of neurologic injury should always be considered in a patient with orbital roof fracture.

Figure 5
Shows a neurosurgeon drilling prior to placing an intracranial pressure monitor.
Shows a neurosurgeon drilling prior to placing an intracranial pressure monitor.
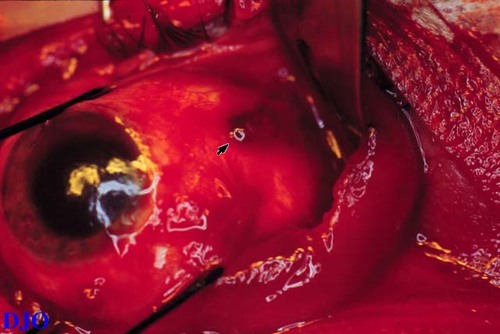
Figure 6
Intraoperative photo of the surgical exploration. The arrow points to a darker area which represents uvea prolapsing through the scleral rupture
Intraoperative photo of the surgical exploration. The arrow points to a darker area which represents uvea prolapsing through the scleral rupture
2) McLachlan DL, Flanagan JC, Shannon GM: Complications of Orbital Roof Fractures. Ophthalmology. 89:1274-1278. (1982)
3) Sullivan WG: Displaced Orbital Roof Fractures: Presentation and Treatment. Plastic and Reconstructive Surgery. 87: 657-661. (1991)