39 year old asymptomatic woman with a history of "glaucoma"
Digital Journal of Ophthalmology 1996
Volume 2, Number 6
October 25, 1996
Volume 2, Number 6
October 25, 1996
PMHx: Non contributory
Meds: Timoptic 0.5% OS BID, Propine OS BID, Pilocarpine 2% OS QID
SHx: Non contributory
FHx: No history of glaucoma
Pupils: No APD
External: Normal OU
Slit lamp examination: The conjunctiva and sclera were white and quiet OU. The corneas were clear OU. The anterior chamber had no cell or flare.
Tonometry: 15 mmHG OD, 38 mmHG OS
Fundus examination: The left disc shows evidence of glaucomatous cupping with a thin temporal rim. The disc, macula, and vessels OD were within normal limits.
Visual Fields: Testing using the Humphrey automated perimeter showed glaucomatous field loss OS. The visual field was normal OD.
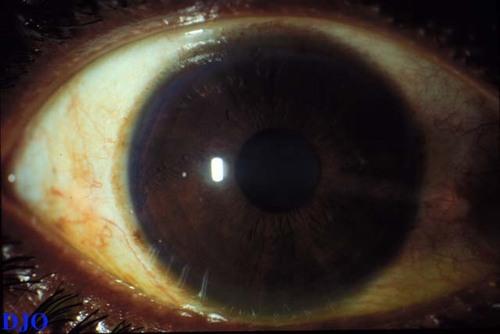
Figure 1
Figures 1-2. These are low magnification photographs of the patient's anterior segments which SHOW distortion of the patient's left pupil (without dilation). The patient's right anterior segment is normal.
Figures 1-2. These are low magnification photographs of the patient's anterior segments which SHOW distortion of the patient's left pupil (without dilation). The patient's right anterior segment is normal.
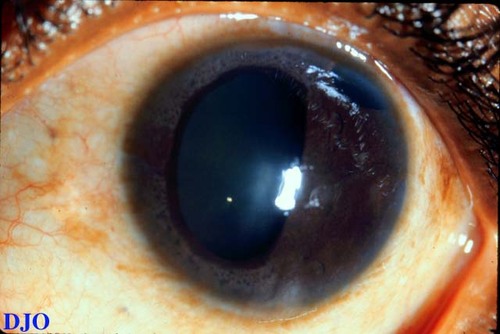
Figure 2
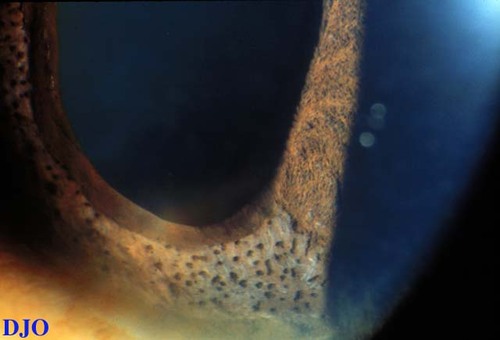
Figure 3
Figures 3-5. Figure 3 and 4 demonstrate multiple fine iris nodules in the patient's left eye. Figure 5 is a gonio-view demonstrating a large area of peripheral anterior synechiae which pulls on the iris and distorts the pupil.
Figures 3-5. Figure 3 and 4 demonstrate multiple fine iris nodules in the patient's left eye. Figure 5 is a gonio-view demonstrating a large area of peripheral anterior synechiae which pulls on the iris and distorts the pupil.
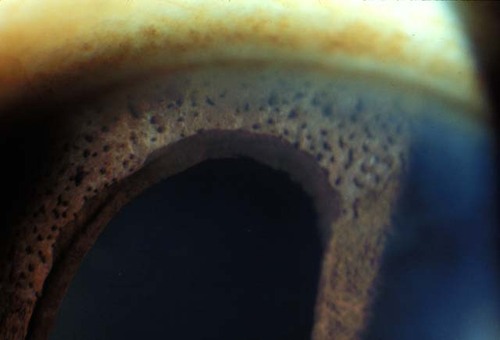
Figure 4
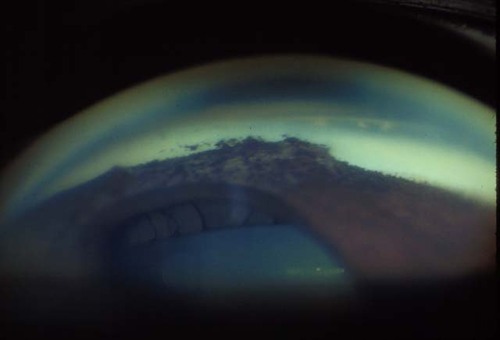
Figure 5
- Axenfeld-Rieger Syndrome
- Iris Nevus Syndrome
- Iris Mammilations
- Chronic anterior uveitis
- Iridocorneal Endothelial Syndrome
The ICE syndrome is a rare uniocular condition which occurs more often in women, is not associated with systemic disease, and which has no obvious genetic predisposition. Onset of the disease usually occurs in early to mid adulthood. The most common presenting complaints include: abnormalities in the appearance of the iris, pain, and decreased vision. On examination these patients often have iris abnormalities and may also have uniocular glaucoma on the same side.
There are several variants of ICE syndrome:
Progressive Iris Atrophy: Atrophy of the iris is present with stretch hole formation due to peripheral anterior synechiae opposite the location of the hole. Secondary glaucoma may be present.
Chandler's Syndrome: This is the most common variant and is charactererized by corneal edema, mild iris changes if any, and normal tonometry.
Cogan-Reese Syndrome: This variant demonstrates iris nodules (as in our patient) that look like nevi. Histologically the nodules are made up of normal iris stroma that has been pinched off at the base by an abnormal corneal endothelial membrane that is spreading over the iris surface. These patients also have peripheral anterior synechiae and angle closure.
Iris-Nevus Syndrome: This should not be considered a variant of ICE syndrome, but can be confused with the Cogan-Reese Syndrome. The "nevi" in iris-nevus syndrome represent true nevi histologically.
Studies have shown that the ICE syndromes represent a spectrum of disease that are linked by a common corneal endothelial abnormality. On slit-lamp examination there is a fine hammered silver appearance of the corneal endothelium and this is a consistent feature found among all of the variants of ICE syndrome. Specular microscopy provides additional information on the endothelial changes. These changes include endothelial cell pleiomorphism, dark areas within cells, and loss of hexagonal margins. These findings when present are essentially pathognomonic for the disease. Characteristically, the endothelium of the unaffected eye is normal. The abnormal corneal endothelial cells in ICE syndrome have apparently lost their contact inhibition and thus are capable of migration. A membrane of endothelial cells may grow over the angle and onto the iris surface to form peripheral anterior synechiae and cause glaucoma. These membranes can also retract and form stretch holes in the opposite quadrant. As a result correctopia, polyopia, and angle closure are often present.
Management of ICE syndrome primarily involves control of the secondary glaucoma and corneal edema. Modalities for treatment of the elevated IOP include medical therapy to suppress aqueous production and filtration surgery. Filtration surgery is often successful early on, but may fail due to endothelization of the fistula by the abnormal corneal endothelium. Miotics and laser trabeculoplasty have not been found to be useful. Corneal epithelial edema may be treated with hypertonic saline. Lowering of the IOP can also be helpful in reducing the amount of corneal edema.
2) M. Bruce Shields and John Bourgeois, Iridocorneal Endothelial Syndrome in The Glaucomas, Chapter 54, p 963-980 (1994)