53 year old female complaining of "seeing blood" OU for 4 weeks
Digital Journal of Ophthalmology 1996
Volume 2, Number 4
October 7, 1996
Volume 2, Number 4
October 7, 1996
PMHx: Hypertension, sickle cell trait
Meds: Lopressor
SHx: Non contributory
FHx: Non contributory
Pupils: Equal, reactive, No APD
Motility: Full OU
External: Normal OU
Intraocular pressure: 16 OU
Slit lamp examination: Normal OU except mild cataracts OU
Dilated fundus examination: See Figures 1-2
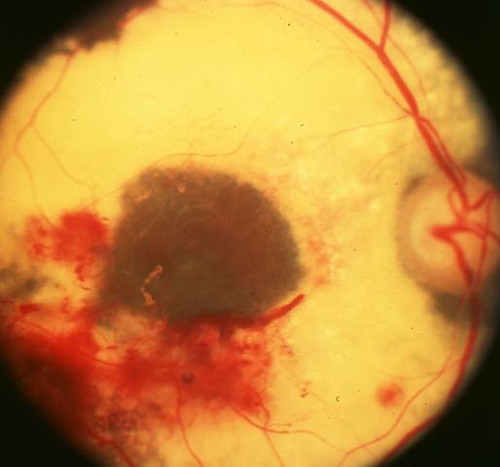
Figure 1
Figures 1-2. Dilated fundus photographs showing extensive exudate, hemorrhages, and microaneursyms.
Figures 1-2. Dilated fundus photographs showing extensive exudate, hemorrhages, and microaneursyms.
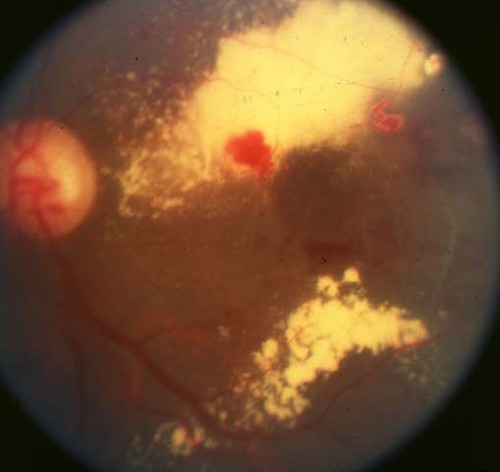
Figure 2
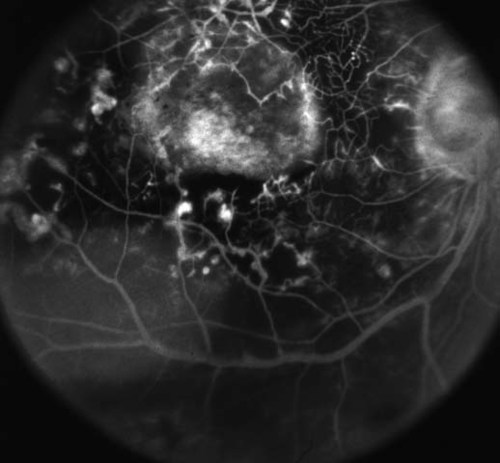
Figure 3
Figures 3-6. Early and late fluorescein angiograms showing extensive microaneurysms, neovascularization, non-perfusion and exudation.
Figures 3-6. Early and late fluorescein angiograms showing extensive microaneurysms, neovascularization, non-perfusion and exudation.
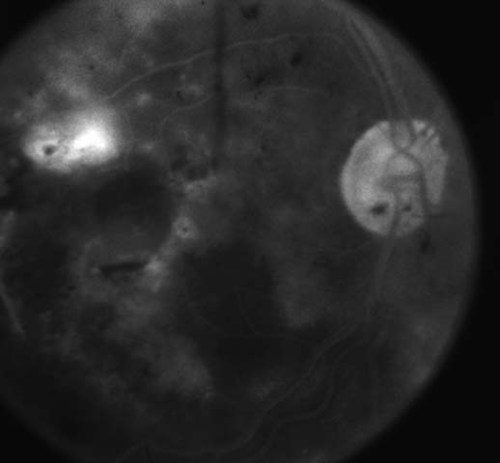
Figure 4
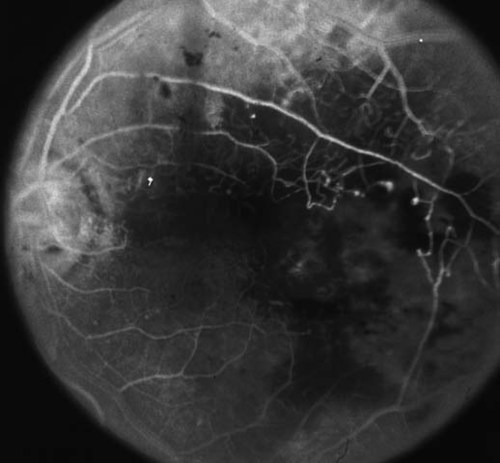
Figure 5
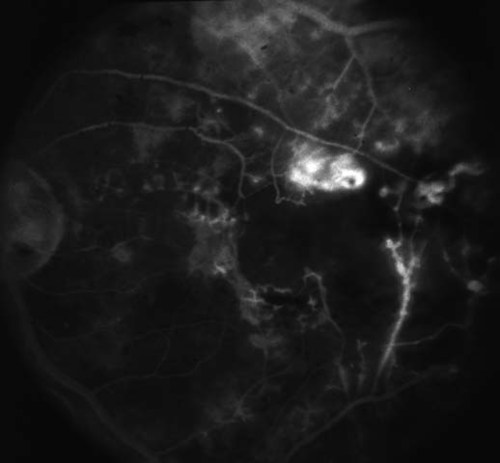
Figure 6
- Diabetic retinopathy
- Radiation retinopathy
- Eale's disease
- Coat's disease
- Sickle cell retinopathy
A review of the patient's chart revealed that she had been seen previously in the Retina Service. The photo chart was pulled and this is how the patient looked 6 years previously. Does this narrow the differential?

Figure 7
Figures 7-8. Dilated fundus photographs showing exudate, preretinal hemorrhages, microaneursyms, and neovascularization.
Figures 7-8. Dilated fundus photographs showing exudate, preretinal hemorrhages, microaneursyms, and neovascularization.

Figure 8
Radiation retinopathy is an occlusive microangiopathy secondary to endothelial cell loss and capillary closure occurring after ionizing radiation treatment. In 1933, Stallard first described retinal inflammation and degeneration with exudates, hemorrhages, retinal pigment epithelium changes, and optic disc edema in patients treated with radon seeds for retinal tumors. Radiation retinopathy has been seen after both radioactive plaque and external beam radiation for ocular, orbital, and intracranial tumors as well as Graves ophthalmopathy.
Radiation retinopathy is slowly progressive and has a delayed onset of months to years after radiation treatment. The severity is dependent on the total dose of radiation, the daily fraction size, the fraction interval, and the volume of retina irradiated. Usual daily fractions of radiation therapy are two to three Gy with a total course ranging FROM 35-72 Gy. The lowest reported dose of radiation to the retina to cause radiation retinopathy is 11 Gy with the usual threshold dose for retinal damage being 30-35 Gy. Photoreceptors are more resistant to radiation, and animal studies have shown damage to rods with 20 Gy and to cones with 100 Gy. Although damage to photoreceptors has been seen, the inner retinal layers and retinal vascular cells are most affected, causing vessel closure and ischemic retinopathy similar to that in diabetic retinopathy.
Radiation retinopathy has been reported within seven months and up to 8.5 years after external beam radiation and between four to 32 months after radioactive plaque therapy. Patients complain initially of blurred vision or floaters. Multiple clinical features are found including:
- Retinal microaneuryms
- Hemorrhages
- Telangectasias
- Capillary dilation
- Cotton-wool spots
- Exudates
- Macular edema
- Capillary closure
- Perivascular sheathing
- Vitreous hemorrhage
- RPE atrophy
- Central retinal artery or vein occlusion
- Traction retinal detachments
- Neovascular glaucoma.
Patients with preexisting vascular diseases such as diabetes, collagen vascular disease, hypertension, or previous chemotherapy have been reported to develope radiation retinopathy at even lower doses of radiation.
Visual loss FROM macular nonperfusion is probably irreversible. Since radiation retinopathy and diabetic retinopathy are clinically and histopathologically similar, treatment has been based on established therapy for diabetic retinopathy. Kinyoun et al in 1988 used focal and grid photocoagulation to areas of clinically significant macular edema with resultant stabilization of vision. They also used panretinal photocoagulation for high-risk neovascularization with regression of new vessels in half of the eyes and no recurrent vitreous hemorrhages at 19-66 months. Furthermore, pars plana vitrectomy was performed in eyes with nonclearing vitreous hemorrhages. Finally, hyperbaric oxygen has also been proposed as a treatment for radiation retinopathy, but its benefit has been unproven and Stanford in 1984 even described a case where it may have even exacerbated the radiation retinopathy.
2) Amoaku WMK, and Archer DB. Fluorescein angiographic features, natural course and treatment of radiation retinopathy. Eye 4:657-667, 1990.
3) Archer DB, Amoaku WMK, and Gardner TA. Radiation retinopathy-clinical, histopathological, ultrastructural and experimental correlations. Eye 5:239-251, 1991.
4) Irvine AR, Wood IS. Radiation retinopathy as an experimental model for ischemic proliferative retinopathy and rubeosis iridis. Am J Ophthalmol 103:790-797, 1987.
5) Kinyoun JL, Chittum, ME, and Wells CG. Photocoagulation treatment of radiation retinopathy. Am J Ophthalmol 105:470-478, 1988.
6) Maguire AM, and Schachat AP. Radiation retinopathy. In Retina Vol 2, Ed: Ryan S. St. Louis. Mosby Co 1994, 1509-1514.
7) Mukai S, Guyer DR, and Gragoudas ES. Radiation retinopathy. In Principles and Practice of Ophthalmology Vol II. Eds: Albert D, and Jakobiec F. Philadelphia:WB Saunders 1994, 1038-1041.
8) Stanford MR. Retinopathy after irradiation and hyperbaric oxygen. J R Soc Med 77:1041-1043, 1984.