21 year old man with blurry vision OD for one week
Digital Journal of Ophthalmology 1996
Volume 2, Number 3
September 23, 1996
Volume 2, Number 3
September 23, 1996
PMHx: HIV+, history of chickenpox in childhood
Meds: Non Contributory
SHx: Non contributory
FHx: Non contributory
Pupils: Normal OU, No APD
External: Slight scarring on the face and trunk in previous areas of rash
Slit lamp examination: Normal OU, anterior chamber and anterior vitreous clear
Fundus examination: see Figures 1-3
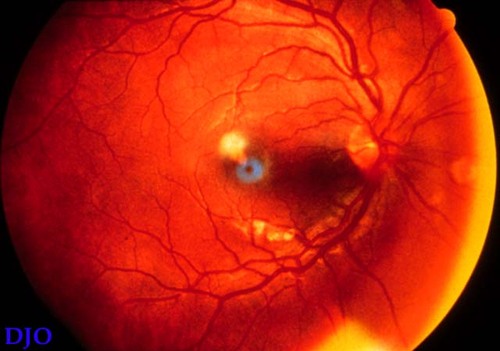
Figure 1
This is a view of the right fundus at presentation, there is a whitish perifoveal lesion in the macula
This is a view of the right fundus at presentation, there is a whitish perifoveal lesion in the macula

Figure 2
View of the right fundus, one week after presentation which shows extension of the whitish lesion, the lesion appears to involve the deep retina with relative sparing of the retinal vessels.
View of the right fundus, one week after presentation which shows extension of the whitish lesion, the lesion appears to involve the deep retina with relative sparing of the retinal vessels.
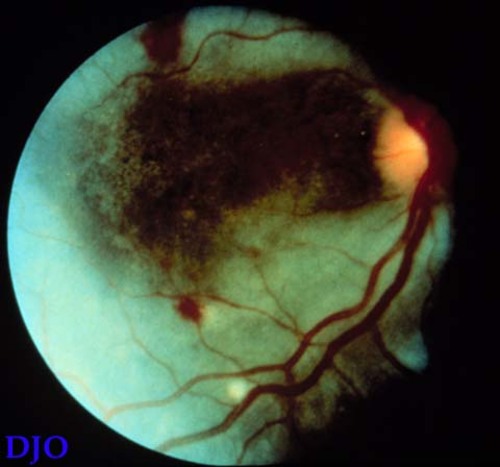
Figure 3
View of the right fundus at four weeks which shows a complete wipe out of the posterior pole by the lesion, there is also a large amount of hemorrhage present. At this point the patient had NLP vision.
View of the right fundus at four weeks which shows a complete wipe out of the posterior pole by the lesion, there is also a large amount of hemorrhage present. At this point the patient had NLP vision.
- Acute retinal necrosis
- Progressive outer retinal necrosis
- Toxoplasma retinitis
PORN is a rare form of necrotizing herpetic retinopathy. It was first described by Forster et al. in 1990, who described two patients with AIDS with unilateral fulminant retinal necrosis involving the outer retinal layers with sparing of the inner retina and retinal vasculature. The majority of patients afflicted with this disorder have been immunocompromised, with al large percentage of those infected with HIV. Engstrom et al in 1994 reported on the largest GROUP of affected patients to date, and in his series all of the patients were male, had a CD4 count of 21, and often had at least one previous AIDS-defining illness. These patients also had an episode of cutaneous zoster (of any dermatome) a mean of two months before onset of visual symptoms.
The pathogenesis of PORN is still elusive, although varicella zoster virus has been postulated to be the causal agent. It has been the ony organism isolated in the retina via culture, polymerase chain reaction, and direct fluorescent antibody assays. the capsids and antigens of the virus have been found in the outer retina of enucleated specimens using immunohistochemical techniques. These discoveries coupled with the close temporal association with cutaneous zoster adds further suspicion that VZV is the causal agent.
Clinical symptoms include unilateral (and sometimes bilateral) subjectively decreased vision, floaters, and loss of peripheral vision. There are no complaints of pain. Objective findings include decreased vision (with a broad range of visual acuity FROM 20/20 to NLP), constriction of visual fields, and in some instances, an afferent pupillary defect. The APD is secondary to relatively uncommon optic nerve involvement, or to asymmetric retinal destruction.
On biomicroscopy, there is minimal intraocular inflammation and several multifocal deep, dense retinal lesions. These lesions progress, and become confluent and full-thickness. As the disease progresses perivenular lucency is seen, which is thought to be due to early clearing of the necrotic debris and and edema. At the end of the disease course, there are areas of dense white plaques that form, giving the retina a Òcracked mudÓ appearance. Atrophic areas with holes can also form after the disease has quiesced. On fluorescein angiography, there are multifocal areas of hyperfluorescence with staining of areas of necrotic retina. There is no leakage or staining of vessels.
Differential diagnoses include primarily the other necrotizing herpetic retinopathies-acute retinal necrosis (ARN) and CMV retinopathy. Acute retinal necrosis is seen mostly in patients who are otherwise healthy. ARN has prominent intraocular inflammation, particularly in the vitreous. There are typically one or more foci of full thickness retinal necrosis with discrete borders. These lesions can be present in the peripheral retina where they involve the major temporal vascular arcades. This entity spreads circumferentially throughout the retina. Other characteristics include pain, scleritis, and optic neuropathy, most often optic nerve atrophy. The visual outcome is much better with ARN than with PORN. The treatment of choice for ARN is acyclovir. CMV retinopathy is a slowly progressive disease with full thickness retinal opacification. The retinal appearance is granular, and often hemorrhagic. CMV also spreads along the vascular arcades, rather than circumferentially, There is a small amount of vitritis present. Initially, the response to antivirals (foscarnet and gancyclovir) is good.
Complications of PORN include rhegmatogenous retinal detachment secondary to atrophic, thin retina with multiple holes. Optic nerve involvement can also occur, presenting as a papillitis or neuroretinitis. Recurrence of disease is the most important complication, occuring so often that most clinicians see it as a normal course of the disease state. The occurrence of new lesions usually occurs at the border of a lesion that has quisced, but can occur in a new area of the same eye or in the contralateral eye. Ultimately 100% of patients of patients who present with unilateral disease progress to have bilateral involvement.
Management of PORN is limited. Antivirals (such as acyclovir and foscarnet) in megadoses have been tried, with limted success in delaying visual loss (20 weeks vs. 4 weeks). However these therapies have not resulted in a better final visual outcome. In one study the final visual acutiy was NLP in 67% of affected eyes within one month of diagnosis. Treatment does not prevent involvement of disease in the fellow eye.
The prognosis for PORN is very poor, as many of these patients lose vision because of retinal detachements, poor response to antiviral therapy, extent of disease, and other factors that are not as yet clearly understood.
2) Forster, David J. et al. Rapidly Progressive Outer Retinal Necrosis in the Acquired Immunodeficiency Syndrome. American Journal of Ophthalmology 110:341 (1990)
3) Laby, Daniel M. et al. Treatment of Outer Retinal Necrosis in AIDS Patients. Graefe's Archives of Clinical and Experimental Ophthalmology 231:271 (1993)
4) Margolis, Todd P. et al. Varicella Zoster Virus Retinitis in Patients With the Acquired Immunodeficiency Syndrome. American Journal of Ophthalmology 112:119 (1991)