A 5-day-old-newborn with a large right upper eyelid coloboma
Digital Journal of Ophthalmology 2017
Volume 23, Number 3
September 28, 2017
DOI: 10.5693/djo.03.2017.08.001
Volume 23, Number 3
September 28, 2017
DOI: 10.5693/djo.03.2017.08.001
Download PDF

Figure 1
Large upper eyelid coloboma in neonatal patient with inferior corneal ulcer and ointment laden corneal surface.
Large upper eyelid coloboma in neonatal patient with inferior corneal ulcer and ointment laden corneal surface.
The tarsus was closed with two lamellar 5-0 absorbable braided polyglactin 910 sutures. The orbicularis was closed with a single 5-0 polyglactin 910 suture. A small amount of redundant cutaneous tissue was excised using a Burrow’s triangle along the relaxed skin tension lines inferolaterally. The eyelid margin was repaired with a vertical mattress 7-0 silk suture, which was then run superiorly to close the skin. The silk suture was removed 2 weeks after surgery. Antibiotic ointment was placed on the surgical wounds.
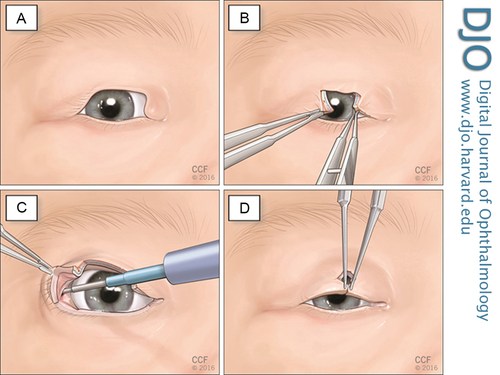
Figure 2
A, Large upper eyelid coloboma B, Edges of the defect are freshened with #15 blade and an initial attempt at direct approximation failed to close the defect. C, The conjunctiva is incised approximately 3 mm superior to the tarsus in the right upper eyelid lateral fornix, and the superior crux of the lateral canthal tendon is lysed with a monopolar cautery instrument. D, The wound edges are precisely anastomosed without undue tension.
A, Large upper eyelid coloboma B, Edges of the defect are freshened with #15 blade and an initial attempt at direct approximation failed to close the defect. C, The conjunctiva is incised approximately 3 mm superior to the tarsus in the right upper eyelid lateral fornix, and the superior crux of the lateral canthal tendon is lysed with a monopolar cautery instrument. D, The wound edges are precisely anastomosed without undue tension.
Correction of large upper eyelid defects in the neonatal period presents unique challenges, because unilateral lid-sharing procedures can result in significant amblyopia. When possible, surgery may be delayed until the age of 3 or 4 years, when more lid tissue is available and the risk of induced amblyopia is decreased.(3) However, especially in larger defects, as in this case, surgery should be performed promptly to lessen or prevent exposure keratopathy. Historically, sliding tarsoconjunctival/myocutaneous flaps,(4) skin grafts,(5) or large lateral myocutaneous flaps(3) have been used with varying success.
In this case, we used internal cantholysis followed by direct closure to repair the large right upper eyelid coloboma. The silk sutures were removed 3 weeks after surgery. A video taken at this time demonstrates excellent eyelid movement and contour (Video 1). At 9 months’ follow-up, there was a favorable eyelid contour, mild ptosis that did not obstruct the visual axis, and very slight lagophthalmos, without noticeable notch formation (Figure 3). There was persistence of superomedial periorbital hollowing, because the severe coloboma also involved the super superomedial fatty tissues in addition to the full thickness of the eyelid. Artificial tear ointment and drops were no longer necessary.
This technique produced significant lid mobility and avoided complications associated with other procedures commonly used for closure of large wounds, such as external scar formation and prolonged occlusion of vision. Although we did not encounter lateral canthal dystopia or lid buckling in this patient, such complications tend to be temporary and improve spontaneously in the early postoperative period.6 In the event that the amount of recruited tissue is initially inadequate, the procedure can easily be converted intraoperatively into a semicircular flap to allow for wound closure. The technique requires minimal equipment, requires no supplementary sutures, and produces excellent cosmetic and functional results, which is especially important in cases with potential for good visual outcome. Internal cantholysis is easily learned and is a powerful technique that should be considered as an option for repairing larger full-thickness lid defects in both adults and children.
Video 1
Patient demonstrating appropriate upper eyelid contour and blink.
Patient demonstrating appropriate upper eyelid contour and blink.
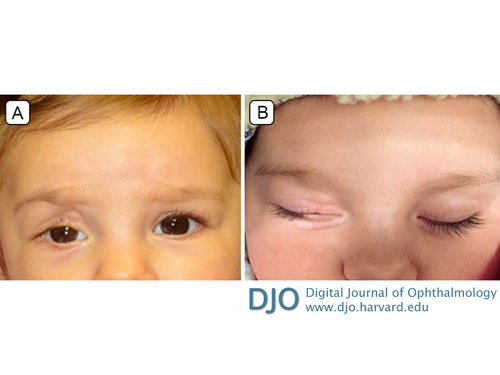
Figure 3
A, Clinical photograph showing appropriate eyelid contour and mild ptosis 9 months postoperatively. B, Trace lagophthalmos without noticeable notch formation.
A, Clinical photograph showing appropriate eyelid contour and mild ptosis 9 months postoperatively. B, Trace lagophthalmos without noticeable notch formation.
2. Mehta MP, Lewis CD, Perry JD. Internal cantholysis for full thickness eyelid defects. Saudi J Ophthalmol 2011;25:31-6.
3. Molina J, Horna E, Miranda A, Rubio R, Larraya A, Casillas G. Congenital upper eyelid coloboma: clinical and surgical management. Case Rep Ophthalmol Med 2015;2015:1-4.
4. Sinkin JC, Yi S, Wood BC, et al. Upper eyelid coloboma repair using accessory preauricular cartilage in a patient with Goldenhar syndrome: technique revisited. Ophthalmic Plast Reconstr Surg 2014.
5. Hashish A, Awara AM. One-stage reconstruction technique for large congenital eyelid coloboma. Orbit 2011;30:177-9.
6. Perry JD, Mehta MP, Lewis CD. Internal cantholysis for repair of moderate and large full-thickness eyelid defects. Ophthalmology. 2013;120:410-4.
7. Tawfik HA, Abdulhafez MH, Fouad YA. Congenital upper eyelid coloboma: embryologic, nomenclatorial, nosologic, etiologic, pathogenetic, epidemiologic, clinical, and management perspectives. Ophthalmic Plast Reconstr Surg 2015;31:1-12.