26 year old female with decreased visual acuity
Digital Journal of Ophthalmology 1999
Volume 5, Number 10
April 8, 1999
Volume 5, Number 10
April 8, 1999
PMHx: Recently diagnosed acute promyelocytic leukemia, otherwise negative
POHx: negative
Medications:
- Allopurinol 300 mg po qd
- Hydroxyurea 1500 mg po bid
- Decadron 8 mg po qd
- Ultransretinoic acid 40 mg po qam, 50 mg po qhs
- Pepcid 20 mg po bid
- Carfate 2 g po tid
SHx: Non-contributory
FHx: Non-contributory
Pupils: Normal (OU), no APD
Motility: Full (OU)
Tonometry: Normal (OU)
External: Normal (OU)
Slit Lamp Examination: Normal (OU)
Fundus Exam: Figures 1-4
Upon presentation three weeks later the patientís visual acuity had improved to 20/25 (OU) and fundus examination revealed that most of the hemorrhages had resolved. The patientís hemoglobin and platelet count had also steadily improved. She was still however being treated for active leukemic disease.

Figure 1
Figures 1-2. Preretinal, intraretinal, and subretinal hemorrhages along with some areas of sub-RPE hemorrhages are present. Mild retinal edema is also present
Figures 1-2. Preretinal, intraretinal, and subretinal hemorrhages along with some areas of sub-RPE hemorrhages are present. Mild retinal edema is also present
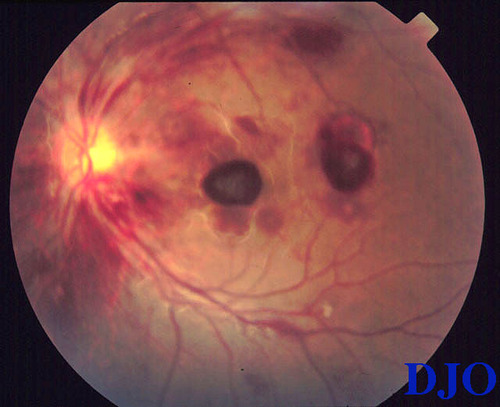
Figure 2
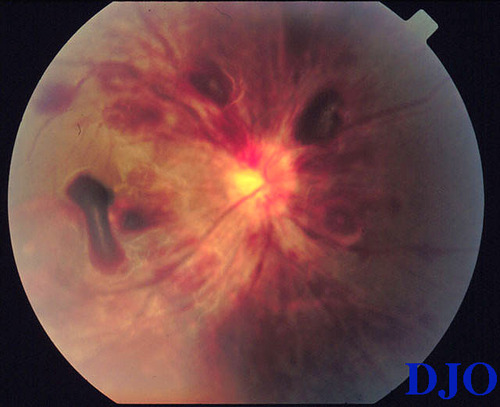
Figure 3
Figures 3-4. Peripapillary never fiber layer and intraretinal hemorrhages are present but the optic nerve is otherwise normal.
Figures 3-4. Peripapillary never fiber layer and intraretinal hemorrhages are present but the optic nerve is otherwise normal.

Figure 4
- Non-proliferative diabetic retinopathy
- Valsalva retinopathy
- Anemic retinopathy
- Leukemia
Transient retinal hemorrhages associated with anemia FROM gastrointestinal hemorrhage were first described by Ulrich(1) in 1883. Subsequently Pagenstecher observed similar examples of retinopathy associated with anemias FROM multiple different etiologies that also resolved upon correction.
The anemias are a GROUP of hematologic disorders manifesting in a decrease in the circulating level of red blood cells and/or a decrease in the level of hemoglobin. Symptoms common to all anemias are weakness and fatigue whereas anemias secondary to specific etiologies may also be associated with particular systemic symptoms.
The manifestations of anemic retinopathy are non-specific and may closely simulate hypertensive or diabetic retinopathy(2). Retinal changes in anemia are common consisting mainly of cotton-wool spots, venous tortuosity, and hemorrhages which may be present at all levels of the retina and choroid. Kanski notes that the duration of the anemia itself does not influence the occurrence of these changes, instead that they seem to be related to the reduction in hematocrit and are more common when the anemia coexists with thrombocytopenia(3).
Factors such as anoxia, venous stasis, angiospasm, increased capillary permeability, and thrombocytopenia have been implicated in the pathogenesis of anemic retinopathy. Other contributing factors include severity of the anemia, increased blood viscosity, as seen in leukemic and other myeloproliferative disorders, and periods of hypotension (especially following severe hemorrhage). The lattermost may also result in shock optic neuropathy which has a presentation and prognosis similar to ischemic optic neuropathy(4). Long-standing anemia FROM Vitamin B12 and/or folate deficiency may also present with optic neuropathy.
Anemic retinopathy has been associated with diseases of the red blood cell elements or as a secondary manifestation of other systemic diseases, and it should be noted that many of the systemic diseases involved may be associated with similar retinal findings exclusive of the anemia per se. Hence, it has been appropriately suggested that since anemic retinopathy is almost always reversible with correction of the anemia, one should be reluctant to ascribe retinal changes entirely to concomitant systemic disease until restoration of normal hemoglobin levels and funduscopic reevaluation(2). As in the case of our patient the retinal findings resolved upon correction of the anemia and thrombocytopenia hence the diagnosis of anemic retinopathy.
2) Weiss, HM. Anemic Retinopathy. Pa Med. 1966. 69(6):35-6.
3) Rubenstein, RA, Yanoff, M and Albert DM. Thrombocytopenia, anemia and retinal hemorrhage. AJO 65: 435, 1968
4) Beck, RW and Smith, CH. Neuro-Ophthalmology: A Problem-Oriented Approach. First Edition. Boston, 1988. Little, Brown, and Company