4 year old boy with proptosis of the left eye and an afferent pupillary defect
Digital Journal of Ophthalmology 1999
Volume 5, Number 9
February 8, 1999
Volume 5, Number 9
February 8, 1999
Past Ocular History: none
Past Medical History: Food allergies to preservatives
Medications: Benadryl p.r.n.
Prenatal History: Delivered at 38 weeks (cesarean section). Mother had toxemia of pregnancy.
Developmental History: No developmental delay
Family History: Non-contributory.
Vision: 20/20 OD, 20/200 OS
Pupils: 2+ afferent pupillary defect OS
Motility: 3 in all fields OD, 1-2 in all fields OS
External: No lymphadenopathy, no sinus tenderness. A soft cystic lesion was palpated in the preauricular region on the left side 2 mm of lagophthalmos
Slit lamp examination: OD: WNL; OS: chemosis, corneal exposure. Otherwise normal
Fundus examination: OD: WNL; OS: opitc nerve head edema, Retinal striae

Figure 1
OS : Severe proptosis, nasal conjunctival chemosis
OS : Severe proptosis, nasal conjunctival chemosis
Pathology
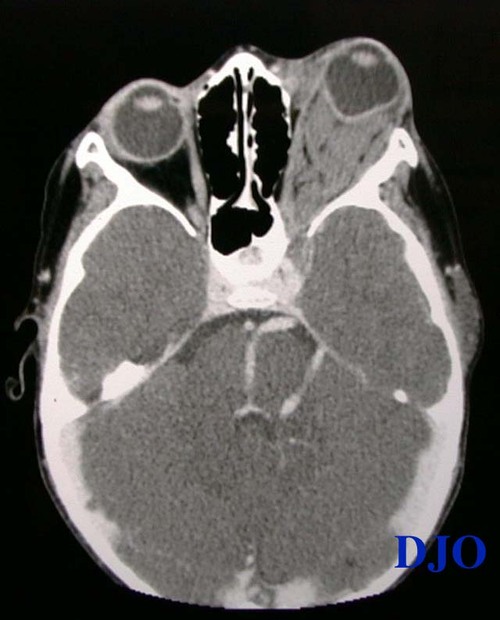
Figure 2
Orbital CT with contrast: Axial: An irregularly-shaped retrobulbar orbital mass filling the posterior orbit with near obliteration of the orbital fat. The severe proptosis and mass effect of the lesion have resulted in an abnormal globe contour. The lesion appears to extend posteriorly through the superior orbital fissure and there is enlargement of the ipsilateral cavernous sinus. A large tortous ipsilateral vascular anomaly is noted. The adjacent paranasal sinuses are clear.
Orbital CT with contrast: Axial: An irregularly-shaped retrobulbar orbital mass filling the posterior orbit with near obliteration of the orbital fat. The severe proptosis and mass effect of the lesion have resulted in an abnormal globe contour. The lesion appears to extend posteriorly through the superior orbital fissure and there is enlargement of the ipsilateral cavernous sinus. A large tortous ipsilateral vascular anomaly is noted. The adjacent paranasal sinuses are clear.
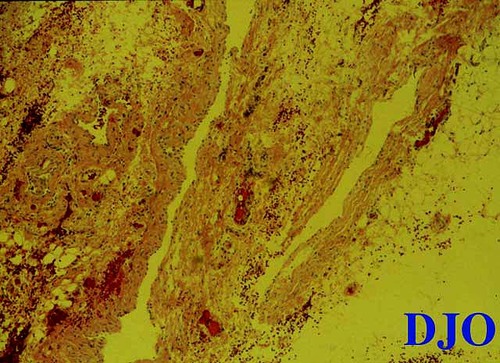
Figure 3
The histopathology is composed of lymph-filled spaces of variable sizes. The spaces are lined by attenuated endothelium characteristic of lymphatic channels.
The histopathology is composed of lymph-filled spaces of variable sizes. The spaces are lined by attenuated endothelium characteristic of lymphatic channels.
The diagnosis of lymphangioma with an acute hemorrhage was highest in our differential. Given the presence of an orbital comparment syndrome (elevated intraorbital pressure resulting INTO an optic nerve compromise) we elected to perform an urgent drainage and biopsy of the mass. The lesion was approached via a lateral orbitotomy following an emergent canthtomy and cantholysis. The mass was found in the intraorbital space, DISTINCT FROM the orbital fat and extraocular muscles. Upon incision of the cystic structure copious amount of venous-appearing blood drained FROM the lesion. Immediately and dramatically the orbit was decongested.
Post-operative report
On post-operative day 1, CT was repeated and an axial image is shown as in Figure 4.
The patient had reversal of his pre-operative afferent pupillary defect, proptosis, extraocular motility limitation. His vision of the right eye was back to 20/25. A focus of nasal chemosis vs. lymphangiectasis had not changed.

Figure 4
Intra-operative photograph showing the "chocolate cyst" caused by the hemorrhage INTO the lesion.
Intra-operative photograph showing the "chocolate cyst" caused by the hemorrhage INTO the lesion.
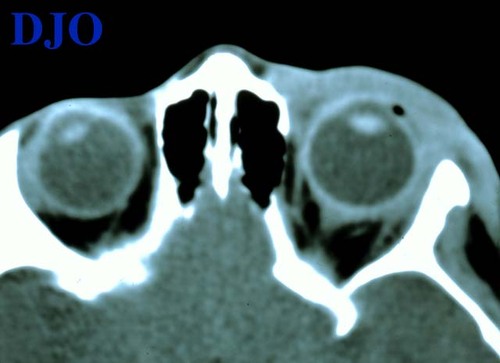
Figure 5
Post-operative (day 1) Axial CT (non-contrast): Significant relief of proptosis, absence of orbital mass, and resolution of globe contour irregularity. Soft tissue changes (edema) in the pre-septal area persisted.
Post-operative (day 1) Axial CT (non-contrast): Significant relief of proptosis, absence of orbital mass, and resolution of globe contour irregularity. Soft tissue changes (edema) in the pre-septal area persisted.
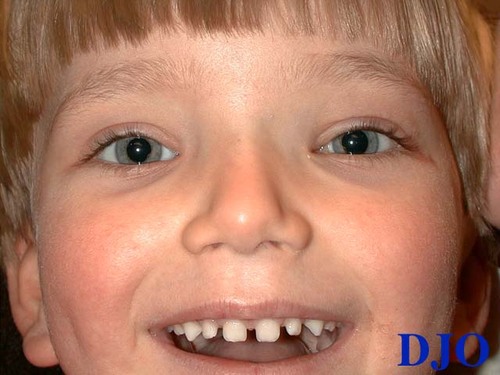
Figure 6
Four months post-operative photo
Four months post-operative photo
- Orbital varix
- Arteriovenous malformation
- Orbital cellulitis
- Capillary Hemangioma
- Cavernous Hemangioma
- Rhabdomyosarcoma
Lymphangiomas are benign vascular tumors that most often appear during the first or second decade of life. These tumors may be found in the conjunctiva, the eyelids, the orbit, or elsewhere in the head and neck region. Spontaneous hemorrhage may be the initial clinical presentation causing sudden exophthlamos and limited eye movement. Most lesions are unilateral and are diagnosed at an average age of six. There is a slightly higher female predilection than males. The lesions are typically diffuse with portions of the lesion interdigitating with normal tissue of the lid and orbit. If located anteriorly, the palpated lesion will feel multilobulated and is easily compressible. There are reports suggesting that the tissue tends to increase in size following an upper respiratory infection, as do other lymphoid structures (tonsils, adenoids, lymph nodes). (1). Trauma may also be a common history to precede the acute hemorrhage. Although some authors believe that this may only be circumstantial given the fact that most of the patients are children and that these are common events in this age group. (2)
Radiologically, lymphangiomas may manifest as a localized mass lesion or as multiple, globular, linear, and bandlike densities within the orbit. There is usually an expansion of the bony orbit on the affected side. Computed tomography shows a cystic component and is characterized with water density and intervening solid tissue with intermediate signal intensity, similar to muscle. The lesions are smooth, contoured, rounded or elongated with multiple, relatively homogenous masses denser than brain. The MR pattern is usually heterogeneous, cysts manifesting as low signal intensity areas on T1 and high signal intensity on T2. The pattern of intensities depends on the fluid composition and the amount and age of hemorrhage. Orbital sonography shows irregular reflectivity, usually with medium-to-low amplitude echoes, and attenuation of the sound beam. Dynamic quantitative A-scanning shows no internal movement to indicate blood flow. Doppler studies reveal no arterial nor venous sounds.
Histopathology: Lymphangiomas have been called choristomas or hamartomas, depending on whether the component vessels are considered to be true lymphatics or dysplastic blood vessels showing some features of lymphatics.(1-3). Histopathologically, they consist of a myriad of irregularly sized and shaped vascular channels with thin walls embedded in a loose fibrous stroma that contains bundles of smooth muscle and collections of lymphocytes. It is an unencapsulated lesion. The vascular channels may be filled with red blood cells or may contain serous fluid, and evidence of old hemorrhage is present in the form of hemosiderin and cholesterol clefts. Thrombosis and calcification may be present. Electron microscopy has shown features of both vascular and lymphatic channels. (3, 4)
Wright suggests that lymphangiomas are hamartomas and renames these lesion as orbital venous anomalies.(5). He feels that lesions posterior to the orbital septum (i.e., within the orbit) are composed of abnormal venous channels. Lesions in the lids and conjunctiva are predominantly venous but there may be associated lymphatic-like vessels as well. He feels that this follows the normal distribution of lymphatics and veins in the orbital tissues.
Katz et al has coined the term combined venous lymphatic vascular malformations (CVLVM). (6). They use this term because of the mixed lymphatic and venous characteristics displayed by these lesions. They have also found frequent associations with noncontiguous intracranial vascular anomalies, which may cause intracranial bleeds. The majority of these lesions have the intracranial involvement on the ipsilateral orbital lesion. They feel that more of these lesions have been undetected because complete intracranial imaging and studies such as magnetic resonance imaging and angiography are not always performed, and sometimes the intracranial anomalies are overlooked. Our patient's findings are most consistent with this variant within the venous malforamtion- lymphangiona spectrum.
Harris et al in a classic paper in 1990 suggested that the lesion is a network of small caliber, malformed vascular channels that arborize irregularly throughout portions of the orbit (2). They too believe that the germ lymphangioma is probably a vascular anlage that has been misdirected by unknown influences, as suggested by Jakobiec and Font (7). They feel that lymphangiomas fall INTO a hybrid category FROM the stand point of their morphologic makings. That is, if vascular anlagen are initially pluripotential, and later more specifically committed, then disruptive influences in different degrees and at different times may produce a spectrum of aberration: the gamut of congenital vascular malformations.
If intervention is necessary, then conservative surgery should be used. Indications for surgery should be limited to acute hemorrhagic episodes causing compromise to the optic nerve, significant corneal exposure, severe discomfort, and the threat of possible amblyopia. Surgical excision of the lesion is not always satisfactory, but most agree it is the treatment of choice. The objective is drainage of the acute hemorrhage and large cystic spaces with their obliteration and excision of as much tumor tissue as possible without jeopardizing normal orbital structures. In one study, 50% of patients had no new hemorrhages after the first surgery. (2). Total excision is rare. Carbon dioxide laser has been shown to facilitate the surgical debulking of lymphangiomas (8). Radical surgery such as exentration of the orbit is not indicated except for severe cosmetic deformity in the presence of a blind eye. Radiation has not shown any role in the management of lymphangiomas.
It is important to emphasize that lymphangiomas cannot be totally excised or "cured", and that each hemorrhagic episode should be managed on the basis of its own functional compromise. The probability of future hemorrhage is highly unpredictable, with or without surgery.
Post-operative report
On post-operative day 1, CT was repeated and the axial image is shown as in Figure 5.
The patient had reversal of his pre-operative afferent pupillary defect, proptosis, extraocular motility limitation. A focus of nasal chemosis vs. lymphangiectasis had not changed.
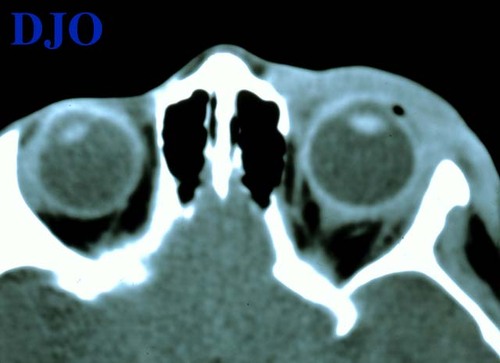
Figure 5 (repeat)
Post-operative (day 1) Axial CT (non-contrast): Significant relief of proptosis, absence of orbital mass, and resolution of globe contour irregularity. Soft tissue changes (edema) in the pre-septal area persisted.
Post-operative (day 1) Axial CT (non-contrast): Significant relief of proptosis, absence of orbital mass, and resolution of globe contour irregularity. Soft tissue changes (edema) in the pre-septal area persisted.
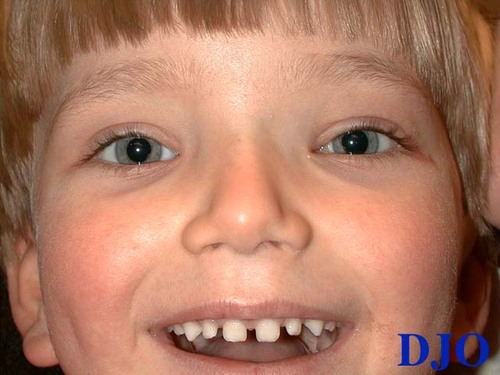
Figure 6 (repeat)
Four months post-operative photo
Four months post-operative photo
2) Harris GJ, Sakol PJ, Bonavolonta G, et al. An analysis of thirty cases of orbital lymphangioma. Ophthalmology 97:1583, 1990.
3) Rootman J, Hay E, Graeb K, et al. Orbital-adnexal lymphangiomas: A spectrum of hemodynamically isolated vascular hamartomas. Ophthalmology 93:1558, 1986.
4) Iwamoto T, Jakobiec FA. Ultrastructural comparison of capillary and cavernous hemangiomas of the orbit. Arch Ophthalmology 97:1144, 1979.
5) Wright JE, Sullivan TJ, Garner A, Wulc AE, et al. Orbital venous anomalies. Ophthalmology 104: 905, 1997.
6) Katz SE, Rootman J, Vangveeravong S, Graeb D. Combined venous lymphatic malformations of the orbit (so-called lymphangiomas): Association with noncontiguous intracranial vascular anomalies. Ophthalmology 105:176, 1998.
7) Spencer WH. Ophthalmic pathology: an atlas and textbook 4th edition. Philadelphia: WB Saunders, 1996;2538-2545.
8) Jordan DR, Anderson RL. Carbon dioxide (CO2) laser therapy for conjunctival lymphangioma. Ophthalmic Surgery 18:728, 1987.