|
|
29 year old woman with loss of visual field in her right eye
Digital Journal of Ophthalmology 1999
Volume 5, Number 8
January 8, 1999
|
Printer Friendly
|
|
|
|
|
|
|
| History |
Presenting History: A twenty nine year old healthy Caucasian female, 8 weeks post-partum, presented with loss of the upper half of visual field in the right eye. The patient noticed blurry vision OD on waking up early in the morning associated with photopsia, lasting 30 minutes which resulted a superior visual field defect. She did not report any improvement in her symptoms when she was seen in the clinic about 9 hours later.
Past Ocular History: none
Past Medical History: Admission in hospital at age of 22 years with severe chest pain which was treated initially as pulmonary embolism. She underwent investigations which did not prove the diagnosis though and the treatment was stopped in a day. No conclusive diagnosis was given for her symptoms.
Past Obstetric History: 3 gravida, 3 para. All the pregnancies were uncomplicated.
Social History: Non-smoker, 2 pints of alcohol a day. |
|
| Examination |
Vision: CF OD improved to 20/20 with raised chin; OS 20/20
Confrontational visual fields: Superior Visual Field restriction, OD; full OS
Pupils: 4 --> 2 OD 4 --> 2 OS
Motility: Full OS
Slit lamp examination: Conjunctiva- white/quite/ no chemosis OU Cornea- clear/quiet OU Anterior chamber- deep/quiet OU Iris- normal, round pupil OU Lens- clear OU
Tonometry: 17 mmHg, OU
Fundi: On dilated funduscopic examination of the right, diffuse whitening of inferior retina of the right eye extending FROM 3 O'clock to 9 O'clock with retinal edema with arteriolar attenuation (Figure 1). No embolus was visible in any retinal arterioles. The left eye fundus was normal.
Goldmanns' Field Test: see Figure 2
FA: Fluorescein angiography was deferred by patient
Hematologic work-up:
"0">
|
Full Blood Count |
All parameters normal |
ESR : |
11mm/ 1 hour |
Auto-antibody screen |
Normal |
Routine Coagulation |
Normal |
Anti Thrombin III |
84 units (75-150) |
Total protein S |
60 units (80-115) |
Protein C |
68 units (70-140) |
Blood Chemistry |
Normal |
Echo Cardiography: Normal
Doppler Carotid Angiogram: Normal
|

Figure 1
Right eye fundus photo on presentation dedmonstrating inferior retinal whitening and edema with arteriolar attenuation
|
|
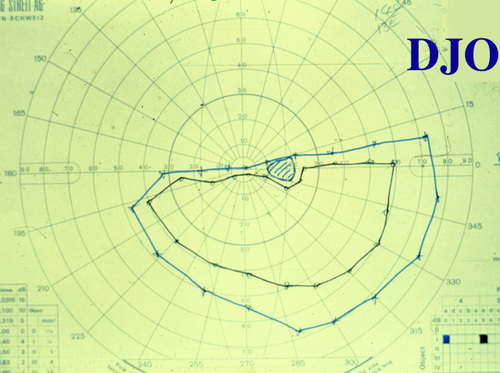
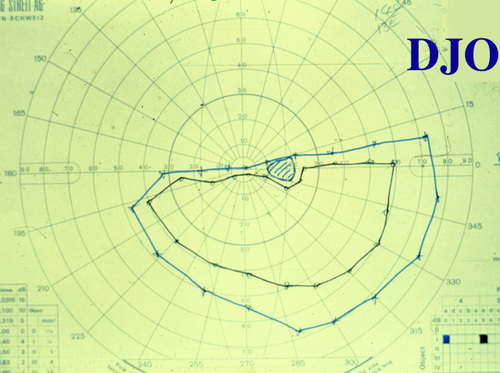
Figure 2
Goldmanns' Visual Field testing demonstrating sharply demarcated superior visual field loss in the right eye
|
|
| Differential Diagnosis |
Differential Diagnosis of BRAO:
- Embolic event
- Hypercoagulable state due to pregnancy
- Systemic disorders i.e. vasculitis, collagen vascular diseases |
|
| Diagnosis and Discussion |
Post-partum Branch Retinal Artery Obstruction
The diagnosis was branch retinal artery obstruction due to protein S and protein C deficiency, presumably induced by pregnancy.
Retinal artery obstruction is rare in young patients. The associated etiologic factors are often diverse and different FROM those underlying artery obstruction in an elderly patient. Patients commonly have various factors leading to hypercoagulable state or embolic conditions. Cardiac valvular disease, history of migraine, hypercoagulable state due to pregnancy, Oral Contraceptive Pill usage, obesity, omocystinuria and hyperhomocytienemia are some of the documented associations. A hypercoagulable state can also be induced by protein S and protein C deficiency and Anti-phospholipid syndromes. Protein C and protein S are vitamin-k dependent anticoagulants. Activated protein C inhibits the clotting cascade by inhibiting factor V and factor VIII. Protein S acts as co-factor in activation of protein C. The deficiency of either factor can be inherited or acquired. An Inherited deficiency is transmitted as an autosomal dominant trait. The deficiency can be acquired in conditions like septic shock, disseminated intravascular coagulation, acute respiratory distress syndrome, post-operative states, liver diseases, pregnancy, Oral Contraceptive Pill use, patients with human immuno-deficiency virus infection and chemotherapy for breast cancer.
The prevalence of inherited protein C and protein S deficiency is 5% to 8% in young individuals with thrombotic events. In 60% to 70% of the patients with inherited Protein C or Protein S deficiency, thrombotic events occur spontaneously, while the rest have some associated risk factors. Homozygous congenital deficiency can result in paediatric venous thrombosis and severe neo-natal purpura.
Deficiencies have been associated with branch retinal vein occlusion, central as well as branch retinal artery occlusion, amaurosis fugax and bilateral disc oedema secondary to dural sinus thrombosis. The protein levels are measured by variety of immunologic and functional techniques. Protein C, protein S, Anti-thrombin III and activated protein C resistance should be included in the laboratory evaluation of young patient with suspected thrombotic event. The last test was not carried out in our patient the plasma level of protein S was definitely suggestive of deficiency, likely to be transient deficiency induced by pregnancy. Indeed the levels returned to normal on repeat testing 8 weeks later. The protein C levels could have been at the lower end of the normal spectrum.
Anti-coagulants and thrombolytic agents are recommended to treat these deficiencies. On detection of pregnancy, the patient with inherited deficiency may be started on heparin. Anabolic steroids such as Danazolol and Stanazolol increase the levels of protein C but do not prevent thrombosis. Anabolic steroids have no role to play in treatment of protein S deficient patient. The patients with acquired transient deficiency can be treated either with oral anti-coagulants or low dose dispersible Aspirin, depending on the severity of the deficiency.
Our patient was treated with low dose Aspirin. Improvement in the visual field was noted on follow-up appointment 8 weeks later.(Figure 3) |
|
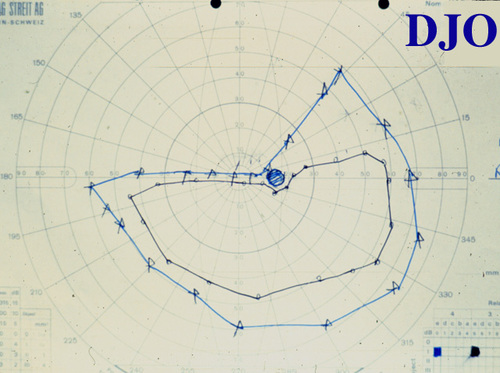
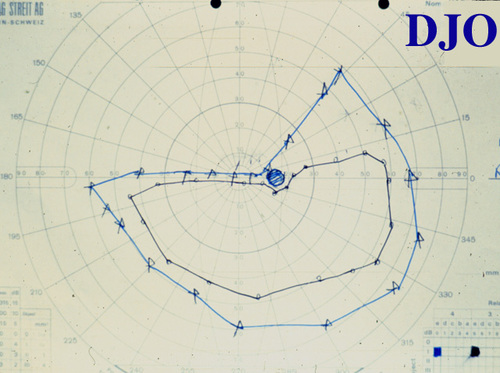
Figure 3
Goldmanns' Visual Field testing demonstrating some recovery of visual field loss in the right eye 8 weeks later
|
|
| References |
1) Craig GM, Madison SM, Richard WG. Retinal Arterial Occlusions in Young Adults. Am J of Ophthalmol, 120:776-783 (1995)
2) Brown GC, Margarel LE, Sheilds JA et.al. Retinal Arterial Obstruction in Children and Young Adults. Ophthalmology, 88:18-25 (1981)
3) Craig GM, Richard WG, Owen J, Madison SM. Protein S Deficiency and Bilateral Retinal Artery Occlusion. Ophthalmology, 98:33-34(1991)
4) Vine AK, Samama MM. The Role of Abnormalities in the Anticoagulant and Fibrinolytic Systems in Retinal Vascular Occlusions, Reviews in Medicine. Surv Ophthalmol, 37:283-292 (1993)
5) Thakaran T, Baxi LV, Diuguid D. Protein S Deficiency in Pregnancy: A case report. Am J Obstet Gynecol, 168:141-2 (1993) |
|