43 year old man presents with blurry vision of the right eye
Digital Journal of Ophthalmology 1998
Volume 4, Number 25
December 8, 1998
Volume 4, Number 25
December 8, 1998
Confrontational visual fields: full
Pupils: 4 --> 2 OD 4 --> 2 OS
Motility: Full OS
Slit lamp examination: Conjunctiva- white/quite/ no chemosis OU Cornea- clear/quiet OU Anterior chamber- deep/quiet OU Iris- normal, round pupil OU Lens- clear OU
Tonometry: OD 22, OS 21
Fundi: On dilated funduscopic examination of the right, a shallow detachment of the macula was seen, with serous subretinal fluid. The optic disk, vitreous, and periphery were normal. Funduscopic examination of the left eye was unremarkable.
FA: Fluorescein angiography was performed. The right eye had multiple RPE window defects and leak points in the perifoveal area.
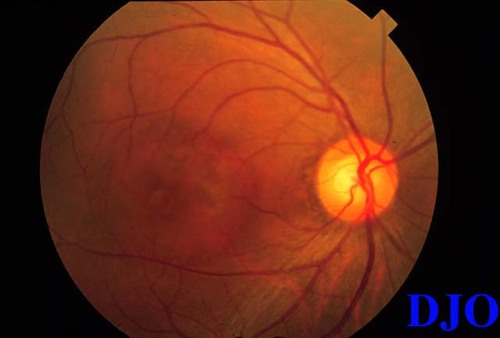
Figure 1

Figure 2a

Figure 2b
- Infections: Histoplasmosis
- Inflammatory conditions: Harada's disease, sarcoidosis,Ê posterior scleritis
- ARMD (must rule out CNV with repeat fluorescein at 2 weeks in patients who present with CSR-like picture who are over 50)
- Retinal holes, optic pits.
This was judged to be consistent with the diagnosis of central serous chorioretinopathy (CSCR).
First described by von Graefe in 1866, CSCR is a disorder afflicting primarily young to middle-aged men (age range: 20-45; 8 fold predominance of men). Association with Japanese & Southeast Asian ethnicity, Type A personality, steroid use, and pregnancy have been reported. Symptoms include a variable decrease in acuity and a range of visual disturbances (micropsia, metamorphopsia, paracentral scotomas).
Examination typically reveals a serous detachment of the macula that is shallow and is accompanied with loss of the foveal reflex. Serous RPE detachments, subretinal precipitates, and RPE atrophy can also occur. A century after von Graefe’s original description, Maumenee & Gass noted the characteristic fluorescein finding of RPE leakage with accumulation of dye within the borders of the detachment. Twenty percent of patients have the classic smokestack pattern, thought to be due to convection currents arising FROM the subretinal fluid HAVING a higher protein concentration than the plasma. Leak points are typically within the 1 mm around the fovea and most frequently in the upper nasal quadrant.
The pathophysiology of CSCR is poorly elucidated. Most theories postulate an insult to the RPE or choroid resulting in a reversal of ion secretion towards the retina. The differential diagnosis is vast, including choroidal tumors, histoplasmosis, and sarcoidosis. Optic nerve pits and retinal holes should be considered if there is no leak point. ARMD with choroidal neovascularization must be ruled out in patients with a CSCR-like presentation who are over 50.
The course is generally benign, with 75-95% of patients achieving a final visual acuity of 20/30 or better. Recurrence occurs in about half of patients. Predictors of poor prognosis include peripheral RPE atrophic tracts, subretinal fibrosis, and diffuse RPE defects. Medical management (beta blockers, acetazolamide, sungazing) are of questionable efficacy. Laser photocoagulation has been shown to decrease duration and recurrence rates. Most studies have found no improvement of final visual acuity with use of laser. Thus, the consensus on use of laser photocoagulation recommends its use in patients who have had no improvement after 3-4 months or those patients who absolutely need optimal vision as soon as possible, e.g., pilots.
2) Khosla, P.K. et al. Evaluation of visual function following argon laser photocoagulation in central serous retinopathy. Ophthalmic Surg Lasers. (1997) 28: 693-7