68 year old man with left orbital fullness
Digital Journal of Ophthalmology 1998
Volume 4, Number 23
October 6, 1998
Volume 4, Number 23
October 6, 1998
PMHx: Longstanding renal failure, chronic sinusitis, coronary artery disease, hypertension, coronary bypass surgery 2 years earlier
Meds: Non-contributory
SHx: Non-contributory
FHx: Non-contributory
Pupils: Normal OU
Motility: Mild restriction to adduction OS
External exam: see Figures 1 and 2
Slit lamp examination: Normal OU
Fundus examination: see Figures 3 and 4

Figure 1
Figures 1-2. Mild proptosis OS with left superonasal orbital mass, which was firm and non-mobile on palpation
Figures 1-2. Mild proptosis OS with left superonasal orbital mass, which was firm and non-mobile on palpation
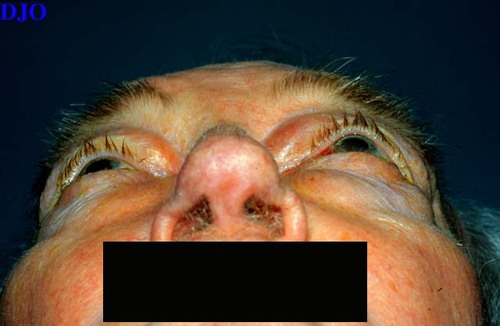
Figure 2
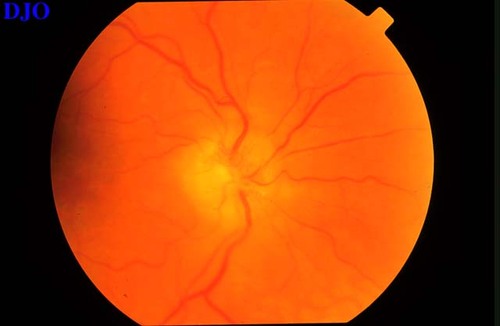
Figure 3
Figures 3-4. Chronic disk swelling OU. Macula and periphery normal OU.
Figures 3-4. Chronic disk swelling OU. Macula and periphery normal OU.
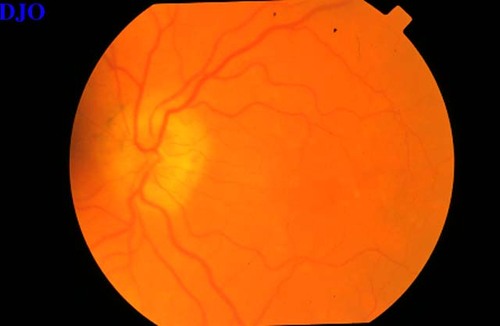
Figure 4
Computed Tomography: see Figures 5-7
Pathology
The patient underwent left orbital biopsy: see Figures 8-9

Figure 5
Figures 5-7. Axial and coronal CT scans showing a space occupying infiltrative lesion extending throughout the medial aspect of the left orbit and extending to infiltrate the meninges of the optic nerve bilaterally in the extra-orbital space.
Figures 5-7. Axial and coronal CT scans showing a space occupying infiltrative lesion extending throughout the medial aspect of the left orbit and extending to infiltrate the meninges of the optic nerve bilaterally in the extra-orbital space.
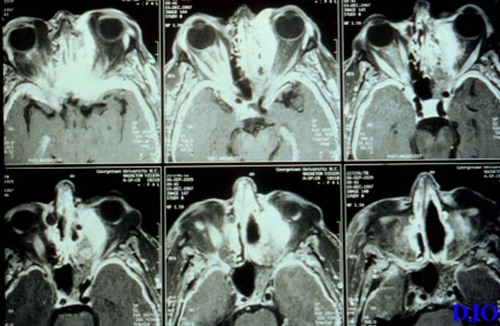
Figure 6
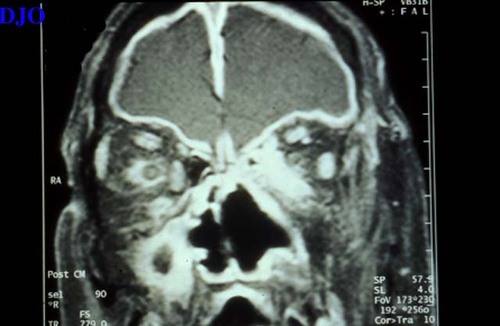
Figure 7
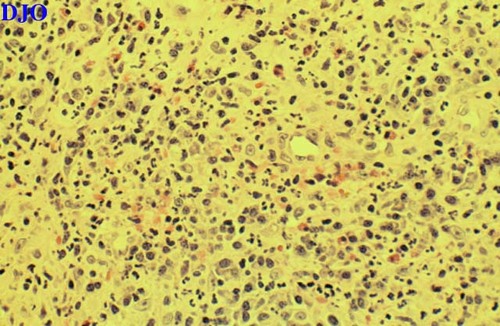
Figure 8
Figures 8-9. Low and high power microscopic views showing necrotizing granulomatous inflammation.
Figures 8-9. Low and high power microscopic views showing necrotizing granulomatous inflammation.
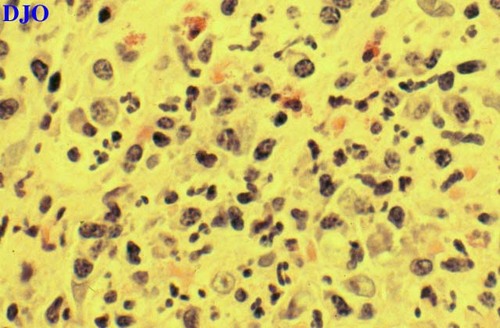
Figure 9
- Pseudotumor
- Wegener's Granulomatosis
- Sarcoidosis
- Aspergillosis
Wegener's Granulomatosis is a systemic disease of unknown etiology characterized by inflammation of the upper and lower respiratory tracts, necrotizing vasculitis and nephritis. It was first described by Wegener in 1936. The disease usually occurs in the fourth to fifth decades of life and is more common in white males. Clinically, the disease can be classified INTO two main categories: generalized and localized.
Generalized Wegener's granulomatosis often manifests with the classic triad of necrotizing granuloma of the upper and lower respiratory tract, vasculitis, and nephritis. All organ systems can be involved. The limited forms of the disease is characterized by necrotizing granulomatous inflammation and vasculitis in the involved tissue. Ophthalmic involvement is present in approximately 50% of patients and is usually divided INTO contiguous disease (arising FROM long standing granulomatous paranasal sinusitis) and focal disease involving the globe itself. Orbital inflammation with proptosis is considered the most common ophthalmic manifestation. This is usually bilateral and causes diplopia, ophthalmoplegia, or orbital apex syndrome. Eyelid granuloma, dacryoadentis, and nasolacrimal duct obstruction have also been reported. Among anterior segment findings conjunctivitis and episcleritis are the most common. Other anterior segment findings include scleritis and peripheral ulcerative keratitis. The posterior segment is rarely involved, but can manifest as retinitis, vasculitis, chorioretinal striae and retinal edema secondary to posterior scleritis. Ocular findings are occasionally the presenting features of the disease.
Pathogenesis of Wegener's Granulomatosis is unclear, but is thought to be immune mediated. Diagnosis depends on the clinical presentation, laboratory testing, and pathology. The C-ANCA blood test is believed to be highly sensitive and specific for this disease. Definitive diagnosis is made by histopathological examination. Typical findings include necrotizing granulomatous inflamation which may be with or without multi-nucleated giant cells.
Treatment relies on the suppression of the immune system with systemic cyclophosphamide and systemic steroid. It is important to note that ocular manifestations of Wegener's need to be treated with systemic immunosuppression.