25 year old man with an acute decrease in vision
Digital Journal of Ophthalmology 1998
Volume 4, Number 22
September 8, 1998
Volume 4, Number 22
September 8, 1998
POHx: myopia and contact lens use
PMHx: Bell's palsy five months ealier which resolved over a two-week period
Meds: none
SHx: Non-contributory
FHx: Non-contributory
Color plates: 12/12 correct OU
Amsler grids: Normal
Confrontational visual fields: full
External exam:
Pupils: 3 --> 2 OD 4 --> 3 OS
Motility: Full OU
Slit lamp examination: anterior segments normal OU
Tonometry: 12mmHg OU
Fundi: Normal disk, vessels and macula OU

Figure 1
Figures 1-2. Automated Humphrey Visual Field of OD and OS. Left inferior quadrantanopsia with superior constriction.
Figures 1-2. Automated Humphrey Visual Field of OD and OS. Left inferior quadrantanopsia with superior constriction.

Figure 2
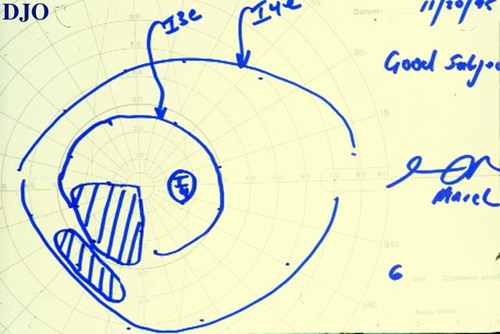
Figure 3
Figures 3-4. Goldmann visual field studies OD and OS. Left inferior quadrantanopsia.
Figures 3-4. Goldmann visual field studies OD and OS. Left inferior quadrantanopsia.
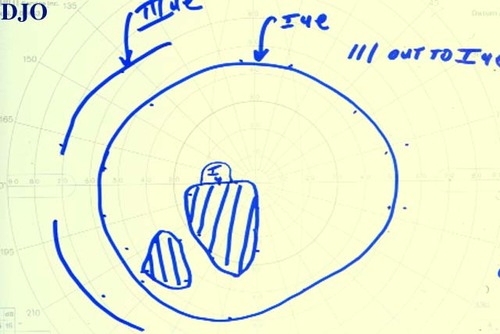
Figure 4
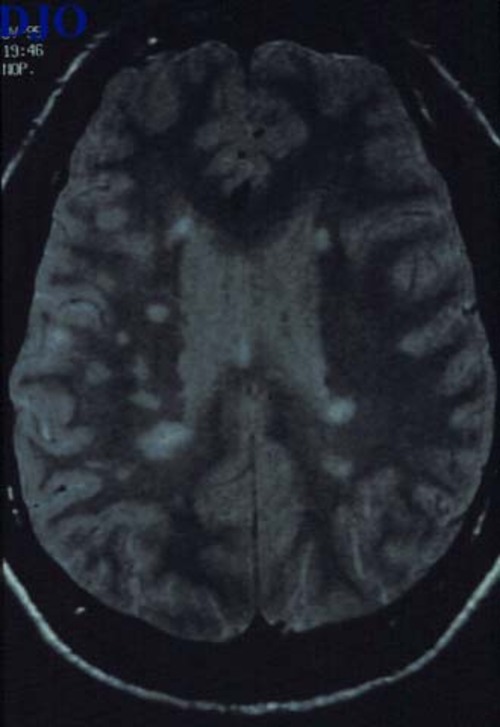
Figure 5
MRI of brain: T2 weighted axial image showing many bright lesions in the periventricular white matter.
MRI of brain: T2 weighted axial image showing many bright lesions in the periventricular white matter.
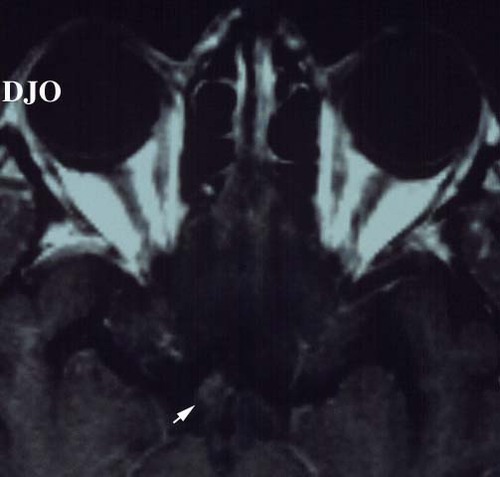
Figure 6
Figures 6-7. Brain MRI: Axial image showing the optic tract: There is enhancement and slight enlargement of the posterior right chiasm and optic tract. Coronal image of the right optic tract also shows enhancement.
Figures 6-7. Brain MRI: Axial image showing the optic tract: There is enhancement and slight enlargement of the posterior right chiasm and optic tract. Coronal image of the right optic tract also shows enhancement.
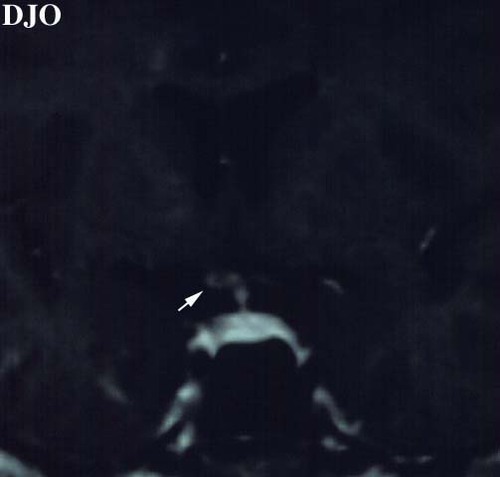
Figure 7
- Embolus to occipital cortex
- Aneurysm
- Tumor
- Demyelination (multiple sclerosis)
Our patient was diagnosed with multiple sclerosis based upon the MRI findings and further review of the patient's history which revealed an episode of numbness in one leg for several weeks and difficulty with the initiation of urination on a separate occasion.
Visual loss in multiple sclerosis (MS) is very common and is the presenting symptom of MS is approximately 25% of patients. Usually, the visual loss is caused by optic neuritis which produces a monocular central scotoma. However, it has long been recognized that homonymoous binocular defects can occur in MS. The earliest report of this was probably by Traquair and was published in the British Journal of Ophthalmology in 1925.
From pathologic and imaging studies it has been SHOW that MS lesions in the retrochiasmal pathways occur frequently. One autopsy study found optic radiation plaques in 85% of patients and a study with magnetic resonance imaging (MRI) also confirmed these findings. However, the prevalence of clinically detectable retrochiasmal lesions in MS is very low. Savitsky and Rangell found no cases out of 415 patients. Hawkins and Behrens found a prevalence of 1.3%. In the largest study with 2000 patients the incidence was 0.9%.
In the literature there are only 26 cases of symptomatic retrochiasmal lesions in MS documented by MRI. Of these patients 64% were women, the average age was 32 and 43% did not have a previous diagnosis of MS at the time of visual loss. Interestingly, 32% of these patients had some degreee of hemiparesis which is unusual in MS.
The visual field findings in these patients was most commonly homonymous hemianopia. Quadrantanopsia was not uncommon and was found in 27% of patients. However, none of the patients in literature with quadrantanopsia had an optic tract lesion as in our patient. 38% of the patients in the literature had highly congruous visual field defects.
The lesions in the 26 patients with MRI studies were most commonly found in the optic radiations. Thirty percent were in the posterior radiations. Thirty-one percent of the lesions involved the optic tract or the lateral geniculate body.
Of the 26 patients in the literature only 2 cases reported treatment. One patient was given oral steroids and the visual field defect resolved after 3 weeks. In another patient I.V. steroids were given and an oral taper. In this patient the visual field defect improved, but was still abnormal at 6 months. In our patient, 4 weeks after presentation the patient had bilateral dyschromatopsia on testing and a left afferent pupillary defect. Six weeks after presentation the patient had resolution of his symptoms and his visual field defect. No treatment was given.
2) Savitsky N, Rangell L: The ocular findings in multiple sclerosis. Assoc Res Nerv Dis Proc 19:403-413 (1950)
3) Hawkins K, Behrens MM: Homonymous hemianopia in multiple sclerosis Br J Ophthalmol 59:334-337 (1975)
4) Plant GT, Kermode AG, Turano G, et al: Symptomatic retrochiasmal lesions in multiple sclerois. Neurology 42:68-75 (1992)
5) Borruat FX, Siatkowski RM, Schatz NJ, et al: Neurology. 43:1430-1432 (1993)