A 64-year-old man with an unusual conjunctival cyst
Digital Journal of Ophthalmology 2017
Volume 23, Number 1
March 8, 2017
DOI: 10.5693/djo.03.2016.04.001
Volume 23, Number 1
March 8, 2017
DOI: 10.5693/djo.03.2016.04.001
Download PDF
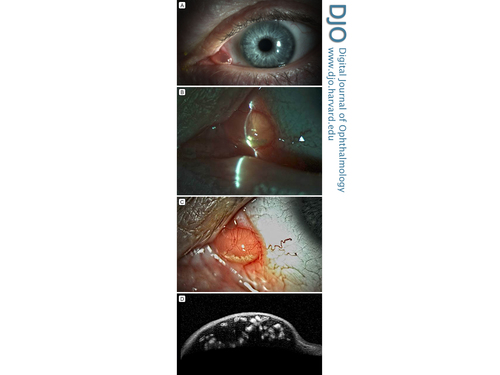
Figure 1
Clinical images. A, Left eye showing conjunctival cyst over the caruncle. B, Transillumination of the conjunctival cyst. C, Enlarged image of the conjunctival cyst. D, Ultrasound biomicroscopy through the inferior border of the conjunctival cyst and intracystic, hyperreflective particles.
Clinical images. A, Left eye showing conjunctival cyst over the caruncle. B, Transillumination of the conjunctival cyst. C, Enlarged image of the conjunctival cyst. D, Ultrasound biomicroscopy through the inferior border of the conjunctival cyst and intracystic, hyperreflective particles.
Histopathological Analysis
Paraffin-embedded, formalin-fixed tissue slides showed a chronically inflamed conjunctival cyst. (Figure 2). Cross-sections of the cyst revealed a degenerating nematode (Figure 2A-C). Sections through the degenerating nematode showed smooth, refractile cuticles, internal lateral ridges, and a suggestion of degenerated internal organs (Figure 2). Pathology images were sent to the Center of Disease Control (CDC), which confirmed the specimen was a nematode but was unable to prove any further classification.
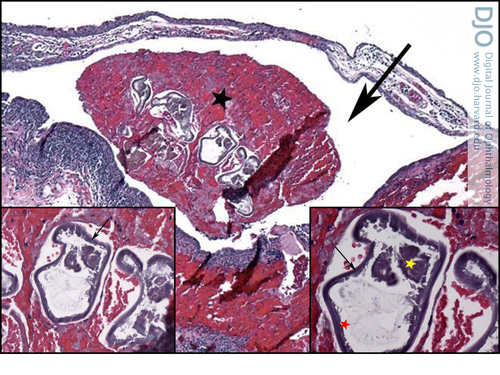
Figure 2
Histopathological analysis (hematoxylin and eosin, original magnification ×4): subconjunctival cyst (black arrow), with degenerating nematode particles (black asterisk). Inset left, higher magnification of the degenerating nematode (×20). Inset right, higher magnification (×40) of the degenerating nematode, with smooth, refractile cuticles (black arrow), internal lateral ridges (red asterisk), and a suggestion of degenerated internal organs (yellow asterisk).
Histopathological analysis (hematoxylin and eosin, original magnification ×4): subconjunctival cyst (black arrow), with degenerating nematode particles (black asterisk). Inset left, higher magnification of the degenerating nematode (×20). Inset right, higher magnification (×40) of the degenerating nematode, with smooth, refractile cuticles (black arrow), internal lateral ridges (red asterisk), and a suggestion of degenerated internal organs (yellow asterisk).
Sebaceous cysts of the caruncle are keratin-filled cysts and can have a yellow appearance, but the intracystic contents are not as mobile on clinical examination as in our patient. Conjunctival lymphangiectasia is another cause for a transparent, cystic-appearing lesion on the ocular surface. This often appears as multiple small bumps on the surface of the eye and occurs when the lymphatic channels in the conjunctiva become dilated and prominent.
Our patient may have been at risk for such an infection due to his interactions with wild animals and possibly due to his time in southern Florida. Dirofilaria tenuis and Dirofilaria immitus are endemic to southern Florida. D. tenuis is also harbored in raccoons in North America.(4) Fortunately, he had an isolated infection and never experienced symptoms or complications from the infection. Since the nematode was already dead, no other treatment was necessary. He was advised to avoid contact with wild animals and it was recommended that he obtain a rabies vaccination. Even if an isolated subconjunctival nematode is alive, surgical removal of the worm is often sufficient.(5) Nematode infections should be considered in patients with unusual behaviors that involve wildlife or if they have migrated from or traveled to endemic areas in the recent past. Thorough systemic evaluation is also recommended.
2. Ashton N, Cook C. Allergic granulomatous nodules of the eyelid and conjunctiva. The XXXV Edward Jackson Memorial Lecture. Am J Ophthalmol 1979;87:1-28.
3. Khoramnia R, Wegner A. Images in clinical medicine: subconjunctival Dirofilaria repens. N Engl J Med 2010;363:e37.
4. Isaza R, Courtney CH. Possible association between Dirofilaria tenuis infections in humans and its prevalence in raccoons in Florida. J Parasitol 1988;74:189-90.
5. Shen J, Gasser RB, Chu D, et al. Human thelaziosis—a neglected parasitic disease of the eye. J Parasitol 2006;92:872-5.