31 year old woman with vertical diplopia for 2 months
Digital Journal of Ophthalmology 1998
Volume 4, Number 21
August 8, 1998
Volume 4, Number 21
August 8, 1998
PMHx: endometriosis, pituitary epidermoid cyst. She reports no unusual birthmarks, no history of prematurity, and no surgery other than that discussed.
Meds: Levothroid, prednisone
Allergies: no known drug allergies
SHx: Non contributory
FHx: Non contributory
Color plates: 10/10 OU
Pupils: OD 4 --> 2 OU, no afferent pupillary defect
Motility: full ductions and versions OU, cover test: exotropia of 8 prism diopters in all directions of gaze.
Neurological Exam: Cranial nerves 1-12 intact
External Exam: see Figure 1
Slit Lamp Exam: anterior segments normal OU, tonometry normal OU
Dilated Fundus Exam: disk, vessels, macula, and periphery normal OU
Goldmann Visual Fields: see Figures 2-3

Figure 1
External photographs of the patient showing right exotropia when the left eye is fixating
External photographs of the patient showing right exotropia when the left eye is fixating
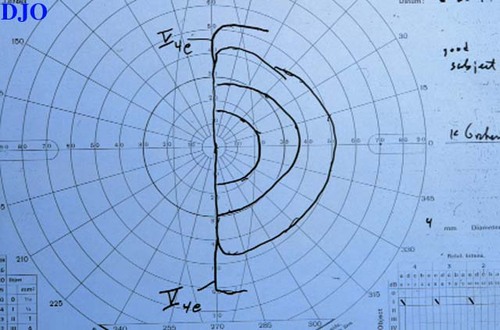
Figure 2
Figures 2-3. Goldman visual fields OU showing dense temporal field loss respecting the vertical midline.
Figures 2-3. Goldman visual fields OU showing dense temporal field loss respecting the vertical midline.
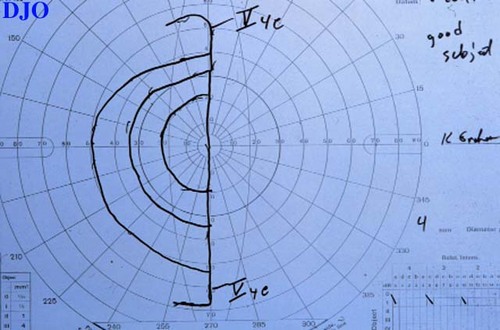
Figure 3

Figure 4
Figures 4-5. Magnetic resonance imaging after the second neurosurgical procedure showing soft tissue swelling but no residual epidermoid cyst or tumor.
Figures 4-5. Magnetic resonance imaging after the second neurosurgical procedure showing soft tissue swelling but no residual epidermoid cyst or tumor.
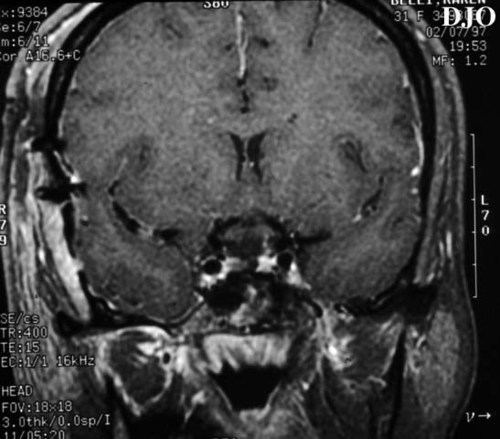
Figure 5
Ocular motor nerve dysfunction: 3rd or 4th cranial nerve palsy, ophthalmic migraine, superior oblique myokymia
Neuromuscular junction disease: Myasthenia gravis, Botulism
Disease of eye muscles: Graves disease, trauma, local anesthesia, chronic progressive external ophthalmoplegia, decompensation of a long standing phoria, metastasis, muscle ischemia (Giant cell arteritis)
Mechanical processes causing vertical eye misalignment: Status post surgery (strabismus, orbital, or retinal), Brown's superior oblique syndrome, pseudotumor, orbital tumors
Retinal disease: Foveal displacement
Other: Fictitious, hemifield slide phenomenon
In 1929, Kubie and Beckmann were the first to describe a transient binocular diplopia associated with bitemporal hemianopic field defects in patients with pituitary tumors without ocular motor paresis. In 1949, Bardram called the phenomenon non-paretic diplopia and described the syndrome in 15 of 90 similar patients. They attributed the problem to damage to the central acuity resulting in attempted perimacular fixation. However, one patient had preserved central acuity in both eyes, as in our patient.
In 1968, Elkington described a series of 260 patients with pituitary adenoma. In 184 of the patients, there was a bilateral temporal defect, of which 84 had a non-paretic diplopia. Elkington was the first to attribute the non-paretic diplopia to problems of "accurately registering the image in each eye."
In 1970, NachtigŠller and Hoyt described how a bitemporal field defect in patients with pituitary masses may experience two types of symptoms. The first is related to depth perception and is referred to as "chiasmatic post fixational blindness." This is related to the loss of the temporal field bilaterally resulting in a blind area beyond fixation. The image posterior to fixation falls on the temporal visual field in each eye and therefore is not able to be seen. As a result, objects in the central vision will disappear when the patient fixates at near, such as with our patient cutting fingernails or threading a needle.
The second GROUP of symptoms was termed "hemifield slide" by Kirkham in 1972. This is related to disruption of ocular fusion and decompensation of a previous phoria. If the eyes intermittently converge, there is a central strip that is not seen. If the eyes have an intermittent exotropia, there will be overlap of the central vertical meridian. A hypertropia will create a misalignment of the two halves of the visual field and produce vertical diplopia.
In 1996, Borchert et al described hemifield slide diplopia FROM altitudinal visual field defects. Two cases of altitudinal defects were described which resulted in the loss of fusion and resulted in separation of the preserved hemifields. One case had a dense inferior altitudinal defect in the field of the right eye and a dense superior altitudinal defect in the field of the left eye. This resulted in the doubling of images vertically. The second case had a partial inferior altitudinal defect in the right eye and a dense superior defect with an inferior island in the left eye. This resulted in episodic binocular vertical and horizontal doubling of images when viewing distant objects.
Clinical Course:
Our patient was given 8 prism diopters as Fresnel prism. The patient reported that this alleviated her diplopia. The prism was then ground in to her glasses.
2) Borchert, M. S., S. Lessell, et al. "Hemifield Slide Diplopia FROM Altitudinal Visual Field Defects." Journal of Neuro-Ophthalmology 16(2): 107-109.(1996)
3) Brazis, P. W. and A. G. Lee "Binocular Vertical Diplopia." Mayo Clin Proc 73: 55-66.(1998).
4) Chamlin, M., L. M. Davidoff, et al. "Ophthalmologic changes produced by pituitary tumors." Am J Ophthalmol 40: 353-368 (1995).
5) Elkington, S. G. "Pituitary adenoma: preoperative symptomatology in a series of 260 patients." Brit J Ophthal 52: 322-328 (1968).
6) Kirkham, T. H. "The Ocular Symptomatology of Pituitary Tumours." Proc R Soc Med 65: 517-518. (1972).
7) Kubie, L. S. and J. W. Beckmann "Diplopia without extra-ocular palsies, caused by heteronymous defects in the visual fields associated with defective macular vision." Brain 52: 317-333. (1929).
8) NachtigŠller, H. and W. F. Hoyt "Stšrungen des Seheindruckes bei bitemporaler Hemianopsie und Verschiebung der Sehachsen." Klin Monatsbl Augenheilkd 156. (1970).