45 year old lady who complained of decreased vision OS of one year duration after cataract surgery
Digital Journal of Ophthalmology 1998
Volume 4, Number 19
June 9, 1998
Volume 4, Number 19
June 9, 1998
PMHx: Non-contributory
Meds: As above
SHx: Non contributory
FHx: Non contributory
Pupils: Equal, reactive, No APD
Motility: Full OU
External: No lid swelling or conjunctival chemosis or injection.
Intraocular pressure: 16 OD, 24 OS
Slit lamp examination: see Figure 1
Dilated fundus examination: Normal OD
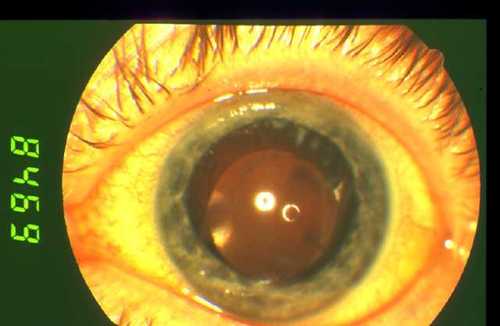
Figure 1
The left eye showed a few cells in the anterior chamber. The anterior segment otherwise showed no obvious inflammation. The cornea and previous incision site looked normal. The pupil was round. A posterior chamber intraocular lens implant was visualised in the capsular bag. There was posterior capsular opacification with a small opening centrally. Peripheral fluffy white spots could be seen superiorly.
The left eye showed a few cells in the anterior chamber. The anterior segment otherwise showed no obvious inflammation. The cornea and previous incision site looked normal. The pupil was round. A posterior chamber intraocular lens implant was visualised in the capsular bag. There was posterior capsular opacification with a small opening centrally. Peripheral fluffy white spots could be seen superiorly.
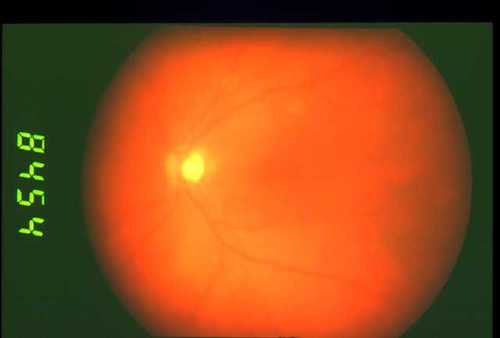
Figure 2
Here is the fundus photo of the patient's left eye. The view was hazy. A few pigmented cells could be seen in the anterior vitreous. The macula looked thickened with binocular fundoscopy, but this is not apparent on the colour photograph. The optic disc was normal.
Here is the fundus photo of the patient's left eye. The view was hazy. A few pigmented cells could be seen in the anterior vitreous. The macula looked thickened with binocular fundoscopy, but this is not apparent on the colour photograph. The optic disc was normal.
Because of the clinical suspicion of cystoid macular edema a fluorescein study was under taken.
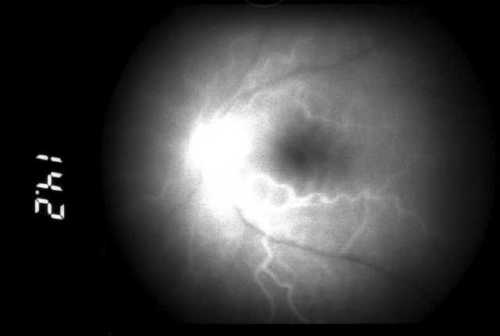
Figure 3
Early phase showing fluorescence in the retinal arteries but no changes in the macula. There is hyperfluorescence and leakage FROM the disk.
Early phase showing fluorescence in the retinal arteries but no changes in the macula. There is hyperfluorescence and leakage FROM the disk.
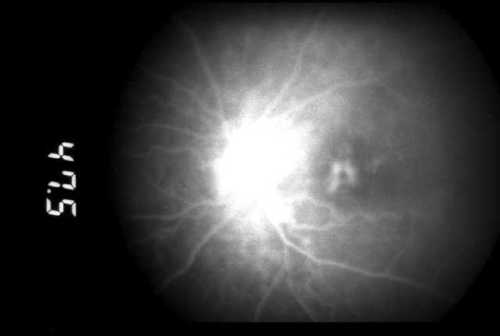
Figure 4
A later phase with pooling of fluorescence in the macular area in a cystic pattern. There is hyperfluorescence and leakage FROM the disk.
A later phase with pooling of fluorescence in the macular area in a cystic pattern. There is hyperfluorescence and leakage FROM the disk.
- Retained lens fragments
- Chronic endophthalmitis
- Auto-immune uveitis (triggered by surgery)
Because of the fluffy white spots on the posterior capsule, there was a suspicion of chronic endophthalmitis FROM an indolent organism. A vitreous biopsy specimen was taken. The intraocular lens implant and capsular bag were removed via a corneal wound and sent for cultures. A pars plana vitrectomy was then performed and the posterior hyaloid face stripped FROM the retina. Subconjunctival cefuroxime and betnesol were given after the procedure.
Bacteriology Results:
Vitreous no organisms on gram stain or culture.
Microscopy/gram staining: fluid FROM IOL and capsular wash showed gram positive cocci.
Overnight culture produced no growth.
Day 6: gram positive pleomorphic rods were seen.
The organisms were sensitive to penicillin, ciprofloxacin and vancomycin, they were resistant to metranidazole.
The cultured organism was identified as Propionibacterium acnes. The patient was started on oral ciprofloxacin and her steroid drops were progressively tapered down.
The patient's post operative corrected aphakic vision is 6/12 in the left eye. The intraocular pressure was 16 mmHg. An anterior chamber secondary lens implantation would be done when the eye showed no more signs of inflammation, with more prolonged follow-up.
P acnes is a gram positive microaerophilic bacillus, a common skin commensal present in the eyelids and ocular surface. The organism can be cultured in thioglycolate media under anaerobic conditions, but this needs to be kept for at least 7 days.(1)
It is known for causing delayed onset pseudophakic endophthalmitis, which is recurrent endophthalmitis due to sequestration of organisms within capsular remnants, where they survive topical, intravenous or even intraocular antibiotics. The endophthalmitis can be worsened by laser capsulotomy. After surgery, residual lens cortex can interact with the bacteria to cause a type of phacoanaphylactic response(2). The present patient is unusual in that the inflammation started immediately after surgery. Also, the large keratic precipitates of granulomatous uveitis, typical of this condition, were absent in this patient.
Previous sporadic cases of this condition has been reported recently.(3-5) A case of anterior chamber intraocular implant surgery associated with this condition has been reported.(6) An outbreak of 4 cases FROM the same surgeon over 2 years have also been reported.(7)
The largest series (22 culture positive cases) has been reported by Winward et al (8). The authors advocated the following approach for post operative endophthalmitis:
Acute cases (within a week of surgery) should be treated with vitreous biopsy and intravitreal antibiotics. These cases are generally not associated with P acnes.
Chronic cases (onset more than one month FROM surgery) can be treated with long term topical steroids if the visual acuity is good and there is minimal intraocular inflammation. Unresponsive cases should be treated surgically by performing pars plana partial capsulectomy (if the full extent of the white plaque is visible); or total capsulectomy through the limbus. The aim of the surgery is to remove all foci of infection. The intraocular lens should also be removed. The authors also favoured an exchange implant in the anterior chamber or in the posterior chamber with transcleral fixation.
Treatment with 100 percent oxygen and infusion of gentamicin and dexamethasone INTO the anterior chamber for 3 patients has been reported.(9) This has been a preliminary report and there is yet no other report of such treatment in the literature.
2) Semel J, Bowe B, Guo A et al. Propionibacterium acnes-enhanced lens-induced granulomatous uveitis in the rat, Invest Ophthalmol Vis Sci, 33(5):1766-70 (1992)
3) Wenkel H, Rummelt V, Knorr H et al. Chronic postoperative endophthalmitis following cataract extraction and intraocular lens implantation. Report on nine patients. Ger J Ophthalmol, 2(6):419-25 (1993)
4) Posenauer B, Funk J. Chronic postoperative endophthalmitis caused by Propionibacterium acnes. Eur J Ophthalmol: 2(2):94-7 (1992)
5) Manners RM, Canning CR. Posterior lens capsule abscess due to Propionibacterium acnes and Staphylococcus epidermidis following extracapsular cataract extraction. Br J Ophthalmol, 75(12): 710-2 (1991)
6) Chien AM, Raber IM, Fischer DH et al. Propionibacterium acnes endophthalmitis after intracapsular cataract extraction. Ophthalmology, 99(4): 487-90 (1992)
7) Rogers NK, Fox PD, Noble BA et al. Aggressive management of an epidemic of chronic pseudophakic endophthalmitis: results and literature survey. Br J Ophthalmol, 78(2): 115-9 (1994)
8) Winward KE, Pflugfelder SC, Flynn HW. Postoperative Propionibacterium endophthalmitis. Treatment strategies and long-term results. Ophthalmology, 100(4): 447-51 (1993)
9) Owens SL, Lam S, Tessler HH et al. Preliminary study of a new intraocular method in the diagnosis and treatment of Propionibacterium acnes endophthalmitis following cataract extraction. Ophthalmic Surg, 24(4):268-72 (1993)