19 year old man with a sore throat, ear pain, and a red eye
Digital Journal of Ophthalmology 1998
Volume 4, Number 18
May 11, 1998
Volume 4, Number 18
May 11, 1998
PMH: None
POH: Myopia, soft contact lens user
Meds: Augmentin, Motrin and Iloticyn
Allergies: NKDA
ROS: Fatigue and malaise lately, possibly fever. No difficulty breathing or productive cough, however, "rib pain" with deep breathing efforts. No joint swelling or tenderness, no back pain and no urethritis.
Visual Acuity: 20/25 OD, 20/20 OS
Pupils: Normal OU
EOM: Full OU.
Color: Normal OU
Exophthalmometry: Normal
Tonometry: Normal OU
Slit lamp examination: see figures 3 and 4
Lids: normal OU
Conjuctiva/Sclera: see figures 3 and 4
Cornea: normal OU
Anterior Chamber: OD:1+ cells OS: normal
Iris: normal OU
Lens: normal OU
Fondus examination: see figures 5 and 6

Figure 1
Figures 1-2. External exam showing swollen tender nose and erythematous painful left earlobe
Figures 1-2. External exam showing swollen tender nose and erythematous painful left earlobe
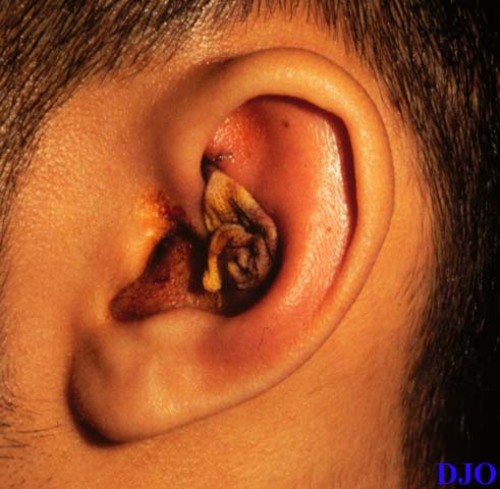
Figure 2
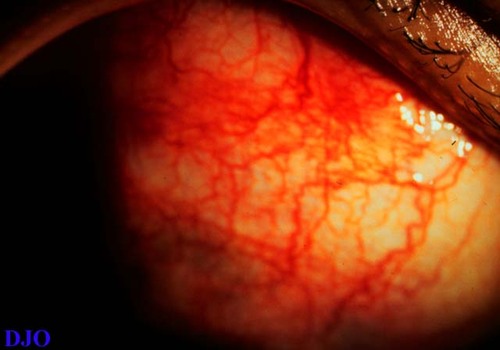
Figure 3
Figures 3-4. There is diffuse scleritis OD (figure 3) and OS is normal (figure 4).
Figures 3-4. There is diffuse scleritis OD (figure 3) and OS is normal (figure 4).
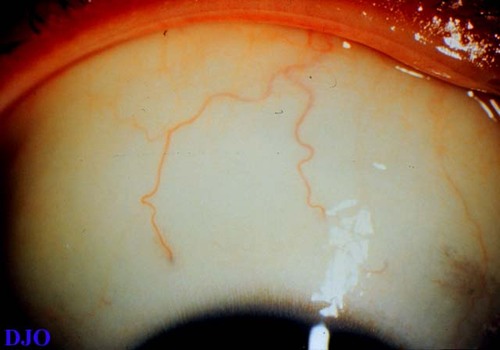
Figure 4
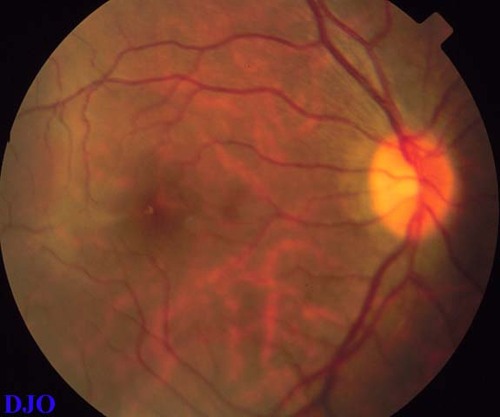
Figure 5
Figures 5-6. Normal funduscopic exams OU.
Figures 5-6. Normal funduscopic exams OU.
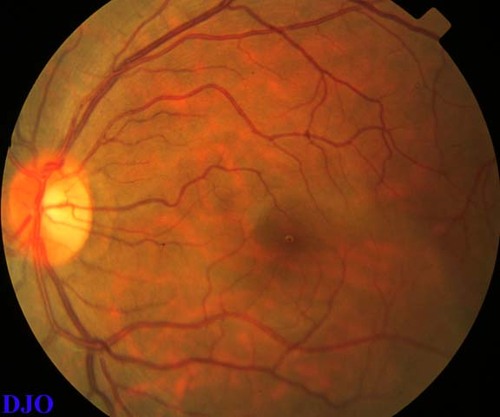
Figure 6
CT scan sinuses and orbits: see figure 7
Chest x-Ray: Normal
Pathology
Nasal Septum Biopsy: Acute non-granulomatous inflammation.
Earlobe Cartilage Biopsy: See figure 8
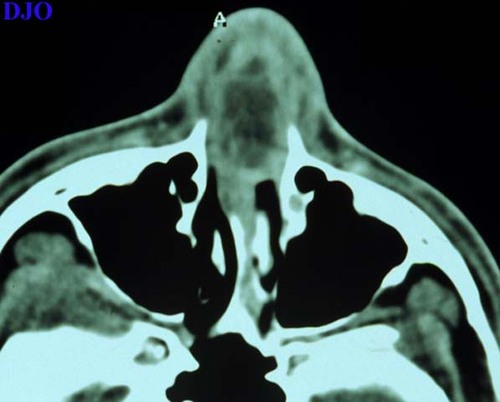
Figure 7
CT scan showing an area of soft tissue swelling in the nasal septum.
CT scan showing an area of soft tissue swelling in the nasal septum.
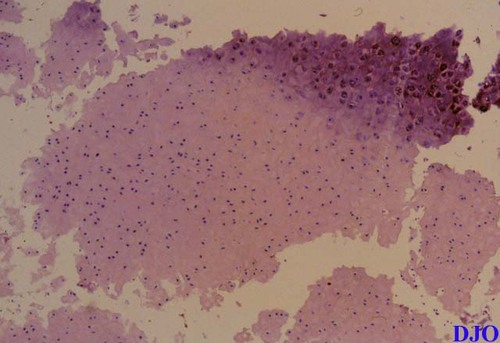
Figure 8
Earlobe cartilage showing loss of basophilic staining of cartilage matrix with some areas of tissue destruction with replacement of fibrous tissue.
Earlobe cartilage showing loss of basophilic staining of cartilage matrix with some areas of tissue destruction with replacement of fibrous tissue.
- Polyarteritis Nodosa.
- Wegener's Granulomatosis
- Infectious Chondritis
- Congenital Syphilis
- Relapsing Polychondritis
General Concepts
Relapsing Polychondritis is a connective tissue disorder of presumably autoimmune etiology, which is characterized by progressive chondritis, ocular, otologic, renal and cardiovascular abnormalities. The median age of onset is 44, with a range of 13-84. It can equally affect males and females, is found in all races, however, it is prominently seen in whites (1). Major clinical features in patients with relapsing polychondritis are (2):
- Chondritis of auricles 90%
- Arthropathy 80%
- Chondritis of Respiratory Tract 55%
- Nasal Chondritis (Saddle Nose Deformitiy) 50%
- Ocular Inflammation 50%
- Cochlear/Vestibular Damage 50%
- Anemia 10%
Detection of autoantibodies to type II collagen (present in cartilage and sclera) and cell mediated immunity to cartilage component in patients with Relapsing Polychondritis suggest an autoimmune mechanism responsible for this disorder (3). Furthermore, immunization of rats with type II collagen induces auricular chondritis similar to that observed in patients with Relapsing Polychondritis (4). Pathological evaluation of affected tissues SHOW perichondrial inflammation, with loss of basophilic staining of cartilage matrix with areas of cartilage destruction with replacement of fibrous tissue.
Diagnosis
There are no laboratory tests that would be specific for this condition. In fact, most of the laboratory work-up is done to rule out other conditions and to determine the involvement of other systems that might be affected, i.e; anemia, renal function, etc. The diagnosis of Relapsing Polychondritis is a clinical one, and is determined by the presence of a combination of clinical findings as determined by the Mc Adam's Criteria revised by Damiani et al (2).
Mc Adam's Signs:
1) Recurrent chondritis of both auricles
2) Non-erosive inflammatory polychondritis
3) Chondritis of nasal cartilage
4) Ocular Inflammation
5) Chondritis of the respiratory tract
6) Cochlear and/or vestibular damage.
Diagnosis of Relapsing Polychondritis:
1) Three or more of McAdam's signs (Histologic confirmation not neccessary).
2) One or more of McAdam's signs with histological confirmation.
3) Involvement of two or more separate anatomic locations with response to steroids or Dapsone.
Ocular Manifestations
Ocular symptoms may be the first manifestation of this disease (1). However, all are non-specific and can be found in other multisystemic inflammatory conditions. Therefore, a high index of suspicions must be maintained.
- Episcleritis 39%
- Scleritis 14%
- Iritis 9%
- Retinopathy 9%
- Muscle Paresis 5%
- Optic Neuritis 4%
- Peripheral Corneal Thinning 4%
Treatment
1) Mild chondritis of auricular, nasal cartilage and arthritis: NSAID.
2) Serious or extensive chondritis and acute respiratory tract involvement: Systemic steroids (Prednisone) and/or Dapsone.
3) Repeated relapses, severe ocular involvement or life-threatening complication, laryngo-tracheal chondritis or glomerulonephritis: Systemic steroids and/or cytotoxic agents.
4) Surgical: Tracheostomy for severe airway involvement.
Scleritis in Relapsing Polychondritis
Scleritis (see figure 9) is a marker of severity of the underlying disease in patients with connective tissue and vasculitic syndromes and is associated with poor prognsois (5). Systemic control of the disease is essential in the treatment of ocular manifestation and immunosuppressive chemotherapy is indicated (6). The following criterias for treatment are suggested:
1) Diffuse Scleritis: Dapsone with or without Prednisone and NSAID.
2) Nodular Scleritis: Azathioprine
3) Necrotizing Scleritis: Cyclophosphomide.

Figure 9
2) J.M. Damiani and Levine, H.L. 1979. Relapsing Polychondritis-Report of Ten Cases. Laryngoscope 89: 929-946.
3) J-M Fiodart, Abe S., Martin, G.R., Zizic, T.M., Barnett, E.V., Lawley, T.J. and Katz, S.I. 1978. Antibodies to Type II Collagen in Relapsing Polychondritis. New Engl J. Medicine. 299:1203-1207.
4) W.J. McCune, Schiller, A.L., Dynesius-Trentham, R.A. and Trentham, D.E. 1982. Type II Collagen-Induced Auricular Chondritis. Arthritis and Rheumatism.. 25:266-273.
5) C.S. Foster, Forstot, S.L., Wilson, L.A. 1984. Mortality rate in rheumatoid arthritis patients developing scleritis or peripheral ulcerative keratitis: effects of systemic immunosuppression Opthalmology: 91:1253-63.
6) T. Hoang-Xuan, Foster, C.S., Rice B.A. 1990. Scleritis in Relapsing Polychondritis. Opthalmology: 97:892-898.