52 year old Filipino female with decreased vision OD for two weeks
Digital Journal of Ophthalmology 1998
Volume 4, Number 17
April 18, 1998
Volume 4, Number 17
April 18, 1998
PMHx: hyperthyroidism
Meds:
SHx: Non contributory
FHx: Non contributory
Pupils: Equal, reactive, No APD
Motility: Full OU
Visual fields: Confrontation fields revealed a relative paracentral scotoma OD, OS was full
External: Normal OU
Intraocular pressure: 14 OD, 16 OS
Slit lamp examination: Normal OU
Dilated fundus examination: See figures 1-3
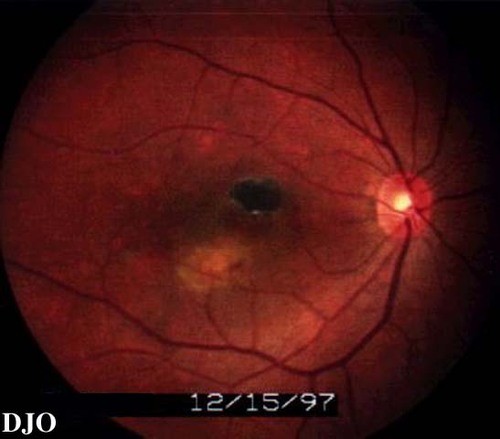
Figure 1
Figures 1-2. Fundus photo OD shows a chorioretinal scar superior to the fovea FROM previous photocoagulation. There is subretinal fluid inferior to the fovea. The choroid has a network of vessels with aneurysm like dilatations.
Figures 1-2. Fundus photo OD shows a chorioretinal scar superior to the fovea FROM previous photocoagulation. There is subretinal fluid inferior to the fovea. The choroid has a network of vessels with aneurysm like dilatations.
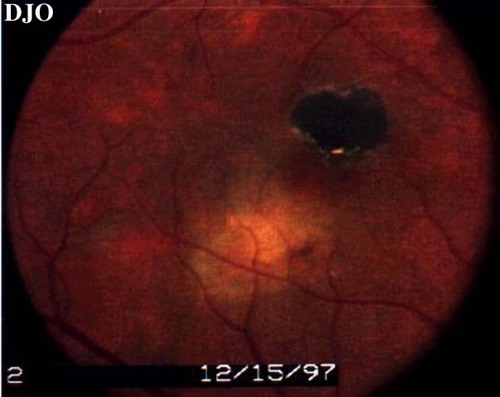
Figure 2
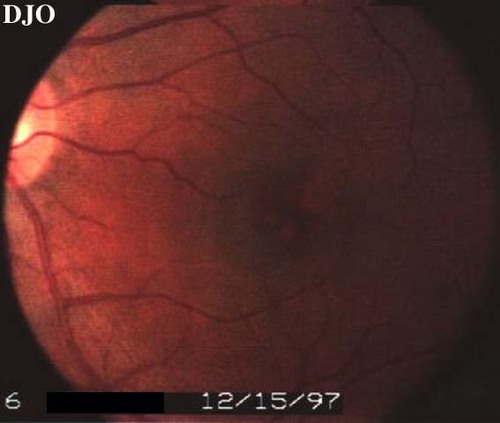
Figure 3
Fundus photo OS shows shows subtle choroidal lesions in the central macula.
Fundus photo OS shows shows subtle choroidal lesions in the central macula.
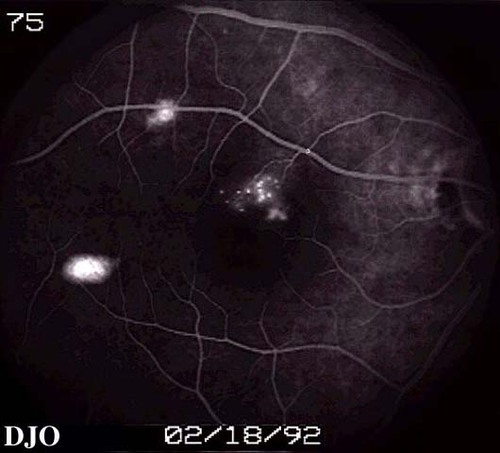
Figure 4
Angiogram of the right eye FROM 1992 shows window defects. Laser photocoagulation had been performed twice before.
Angiogram of the right eye FROM 1992 shows window defects. Laser photocoagulation had been performed twice before.

Figure 5
Red free photo of the right eye shows scar and subretinal fluid. Also note the gray streak-like lesions in the choroid peripherally.
Red free photo of the right eye shows scar and subretinal fluid. Also note the gray streak-like lesions in the choroid peripherally.

Figure 6
Laminar venous phase angiogram of OD shows blocked fluorescence FROM the scar, hyperfluorescent lesion inferior to the fovea, and peripheral hyperfluorescence corresponding to the streak-like gray choroidal lesions.
Laminar venous phase angiogram of OD shows blocked fluorescence FROM the scar, hyperfluorescent lesion inferior to the fovea, and peripheral hyperfluorescence corresponding to the streak-like gray choroidal lesions.
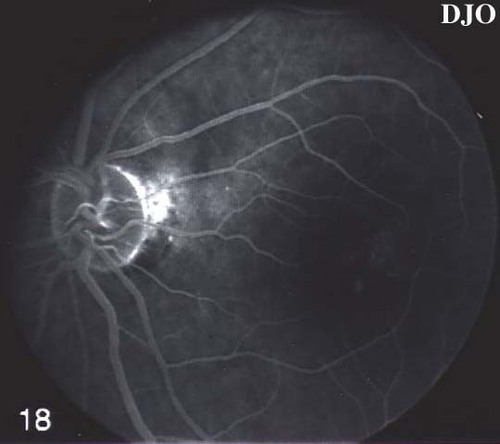
Figure 7
Angiogram of OS shows hyperfluorescence in the macula.
Angiogram of OS shows hyperfluorescence in the macula.
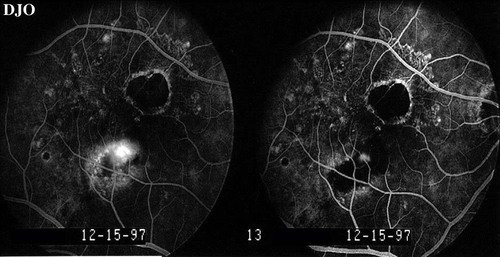
Figure 8
The lesion in the right eye was treated with laser photocoagulation. Acuity improved to 20/40 FROM 20/50. This figure shows the followup angiogram. There is still some leakage INTO the lesion which was retreated.
The lesion in the right eye was treated with laser photocoagulation. Acuity improved to 20/40 FROM 20/50. This figure shows the followup angiogram. There is still some leakage INTO the lesion which was retreated.
ARMD is most often seen in white patients. ItÕs incidence increases with age and a diagnosis of ARMD before age 55 may be some other entity. Drusen and retinal pigment epithelial changes are often seen before the development of exudative features. The vessels of the choroidal neovascular complex are not visible clinically and there is a grey-green discoloration of the membrane. With natural progression there is often a subretinal scar formation. Visual acuity is slowly reduced in the atrophic form of the disease. The exudative form of the disease causes rapid decline in vision.
Idiopathic Polypoidal Choroidal Vasculopathy:
Typically seen in darker skinned individuals; often females in 5th decade onward. Serosanguineous retinal detachments are seen in association with a network of choroidal vessels with polypoid excrescences. Visual acuity is typically good and improves with treatment. There is no associated drusen or scarring.
Central Serous Retinopathy:
Usually seen in males in the third to fifth decades. There is a serous detachment of the retinal pigment epithelium and sometimes the sensory retina. Angiography may SHOW an area of leakage FROM the RPE. There may be an association with steroid use.
Idiopathic Polypoidal Choroidal Vasculopathy has also been called the posterior uveal bleeding syndrome and multiple recurrent serosanguineous RPE detachments in Black women. IPCV typically affects women in their fifth to seventh decades. Darker skinned individuals are affected more than Caucasians. There is no association with features seen in high myopia (lacquer cracks), ARMD (soft drusen), or ocular inflammation. IPCV is usually bilateral.
There are two characteristic findings. A sub RPE branching network which is usually below the papillomacular bundle but can be isolated below the fovea, as demonstrated in the left eye of this case. Reddish-orange nodules, called choroidal excrescences, are found at the edge of the networks.
Recurrent exudation and hemorrhage can occur under the RPE or retina. Breakthrough bleeding INTO the vitreous is possible. Over time, the orange mass like lesions flatten with resolution of the PED. New tubular vessels emanate FROM the flattened orange lesion.
Fluorescien angiography shows filling of IPCV lesions with the choroidal vasculature. There is blocked fluorescence due to hemorrhage, exudate or the RPE. IPCV vessels can leak, though not as much as in a choroidal neovascular membrane seen in ARMD. The polypoid structures are hyperfluorescent and stain or leak on late frames.
Indocyanine green angiography shows that IPCV vessels fill slower than choroidal vessels. The network of abnormal vessels is also larger than suspected clinically. The polypoid structures leak dye slowly.
Vision is typically better in IPCV than in ARMD and vision can be improved with treatment of the lesions. In some cases, scarring can occur with attendant visual loss. Treatment is carried out to areas of leakage FROM the choroidal excrescences.
IPCV can be differentiated FROM ARMD in the following ways. ARMD patients are usually Caucasian. They usually have typical drusen and RPE changes which are often bilateral. The vessels seen in CNV due to ARMD are not clinically visible. There is frequent scarring.
2) Yannuzzi, LA; et. al. Idiopathic Polypoidal Choroidal Vasculopathy (IPCV), Retina. 10:1-8, 1990.
3) Spaide, RF. ICG Videoangiography of Idiopathic Polypoidal Choroidal Vasculopathy,Ó in Yannuzzi, LA; Flower, RW; Slakter, JS; Indocyanine Green Angiography, Mosby, 1997.