52 year old man with intermittent proptosis
Digital Journal of Ophthalmology 1998
Volume 4, Number 16
March 18, 1998
Volume 4, Number 16
March 18, 1998
POH: None
PMH: Sinusitis
Meds: Ibuprofen
Social Hx: Born in Haiti
Family Hx: Non-contributory
Vision: 20/50 OD, 20/20 OS
Pupils: Normal OU
Motility: Moderate to severe limitation in all directions OD, worst on upgaze. Full OS.
Color: Normal OU
Exophthalmometry: 7 mm proptosis OD
External exam: See figure 1
Slit lamp examination: OD: There was 2+ conjunctival injection and a few SPK. The anterior chamber was deep and quiet. The iris and lens were normal. OS: Normal.
Applanation pressures: 16 mmHg OD, 12 mmHg OS.
Fundus examination: See figure 2

Figure 1a
Figures 1a-1b. External exam showing the right eye is displaced inferiorly, injected, and with marked proptosis (7 mm). Also note that motility is decreased as seen here on left gaze.
Figures 1a-1b. External exam showing the right eye is displaced inferiorly, injected, and with marked proptosis (7 mm). Also note that motility is decreased as seen here on left gaze.
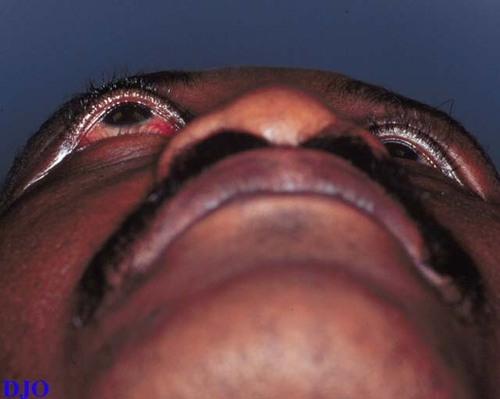
Figure 1b

Figure 2a
Figure 2a-2b. Ophthalmoscopy (Left) Posterior pole OD, showing macular striae and choroidal folds. (Right) Nasal fundus OD, showing areas of elevation consistent with choroidal effusions. The fundus OS was normal.
Figure 2a-2b. Ophthalmoscopy (Left) Posterior pole OD, showing macular striae and choroidal folds. (Right) Nasal fundus OD, showing areas of elevation consistent with choroidal effusions. The fundus OS was normal.
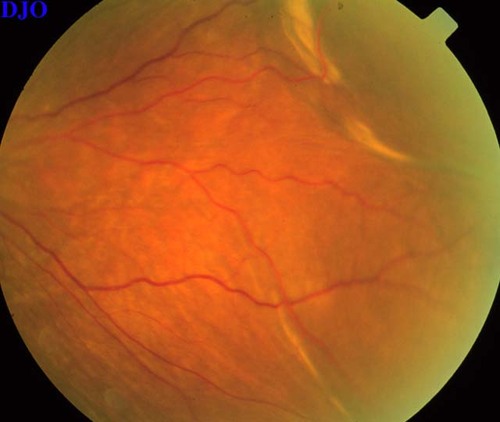
Figure 2b
WBC: 6400 (normal differential)
ESR: 45
Thyroid Function: Normal
ANA: Normal
ACE: Normal
ANCA: Normal
CXR: Normal
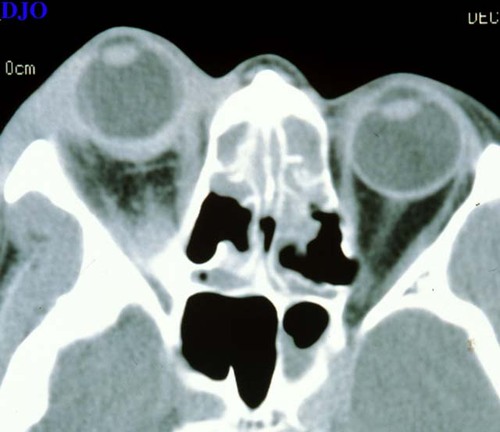
Figure 3a
Figures 3a-3b. Orbital CT (Left) Axial, showing periorbital soft tissue swelling, thickening of the posterior sclera, choroidal elevations, and proptosis OD. (Right) Coronal, showing thickening of the extraocular muscles OD.
Figures 3a-3b. Orbital CT (Left) Axial, showing periorbital soft tissue swelling, thickening of the posterior sclera, choroidal elevations, and proptosis OD. (Right) Coronal, showing thickening of the extraocular muscles OD.

Figure 3b
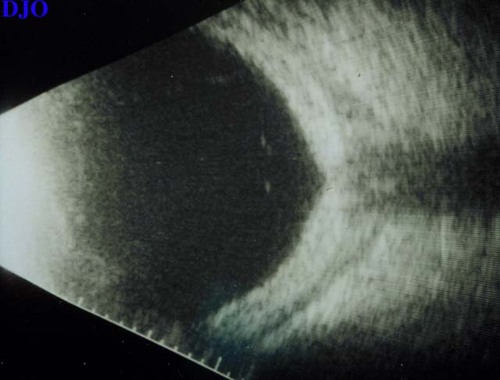
Figure 4a
Figures 4a-4b. B-scan ultrasound (Left) Posterior, showing a sub-tenon's effusion at the junction of the optic nerve and globe (T-sign). (Right) Temporal, showing an exudative choroidal effusion and a sub-tenon's effusion.
Figures 4a-4b. B-scan ultrasound (Left) Posterior, showing a sub-tenon's effusion at the junction of the optic nerve and globe (T-sign). (Right) Temporal, showing an exudative choroidal effusion and a sub-tenon's effusion.
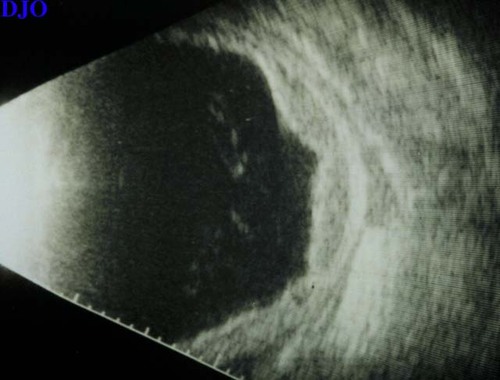
Figure 4b

Figure 5a
Figures 5a-5h. Left column, before treatment. Right column, after 2 weeks of steroid treatment.
Figures 5a-5h. Left column, before treatment. Right column, after 2 weeks of steroid treatment.

Figure 5b
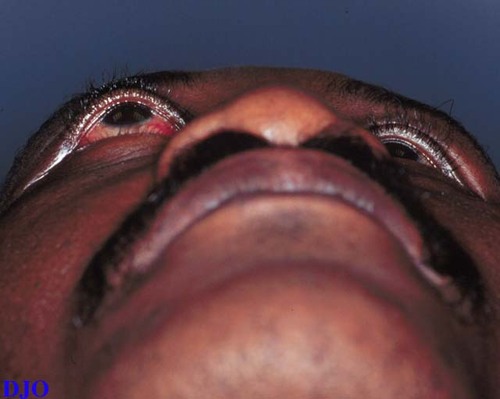
Figure 5c
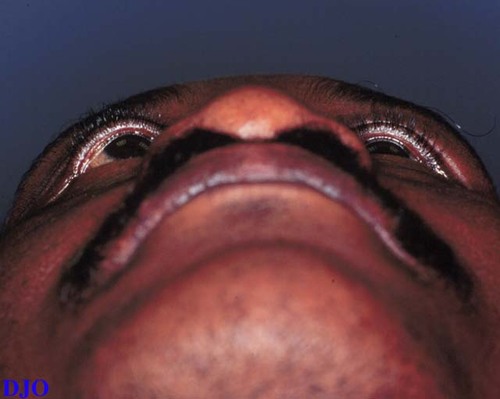
Figure 5d
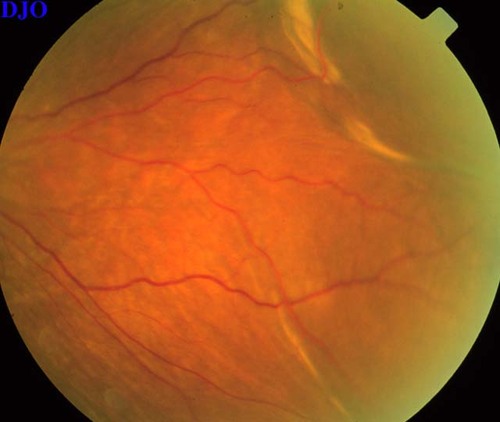
Figure 5e
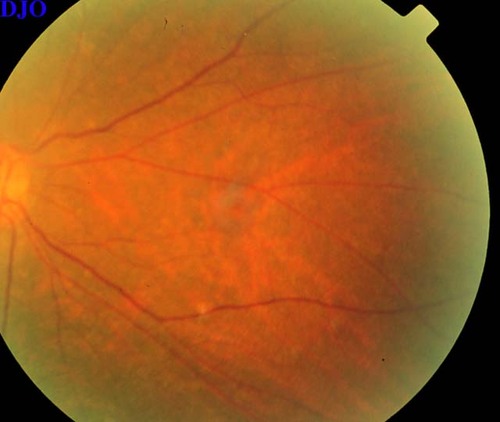
Figure 5f
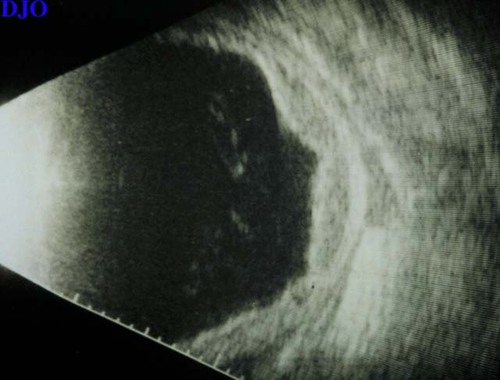
Figure 5g
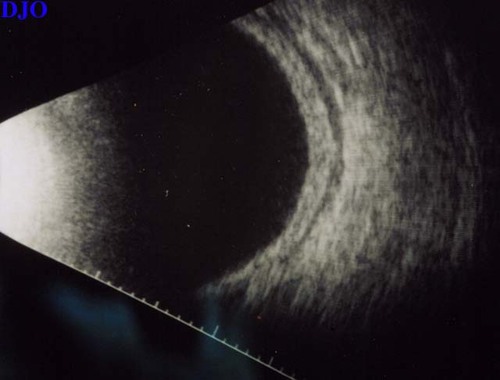
Figure 5h
- Orbital vasculitis: polyarteritis nodosa, Wegener's granulomatosis, temporal arteritis
- Granulomatous disease: sarcoidosis
- Orbital pseudotumor
- Graves' orbitopathy
- Vascular abnormalities: carotid-cavernous sinus fistula, varix
- Orbital tumors: primary, secondary, metastatic
Orbital pseudotumor is a benign idiopathic inflammatory process involving the structures in the orbit which may present in several different patterns. It may be acute, subacute, chronic, or is rare cases recurrent. It may diffusely involve the entire orbit or present in a localized fashion involving either the anterior orbit, posterior orbit, lacrimal gland, or extraocular muscles. Most cases are unilateral, but bilateral cases are seen and are more common in children.
The clinical signs and symptoms vary depending upon the involved tissues. Our patient's presentation was most consistent with acute anterior orbital pseudotumor which typically involves the globe, tenons capsule, sclera, and periscleral tissues. Signs and symptoms of anterior pseudotumor include pain, redness, lid swelling, proptosis, decreased acuity, and diplopia. Uveitis, choroidal effusions, macular edema, papillitis, and increased intraocular pressure may also be seen. Anterior orbital pseudotumor may be difficult to distinguish either clinically or radiographically FROM posterior scleritis as seen in this case and some feel that these two entities may represent the same inflammatory process.
Posterior orbital pseudotumor involves the orbital apex and may present as an optic neuropathy with visual field defects, dyschromatopsia, and an afferent pupillary defect. It may also present as an ophthalmolegia. Orbital myositis involves either single or multiple extraocular muscles and presents with pain on eye movement, diplopia, and proptosis. Acute dacryoadenitis may present as ptosis with swelling of the lateral upper lid.
The diagnosis of orbital pseudotumor is one of exclusion. In an acute presentation, one must first rule out an infectious process. In our case, the patient had a normal WBC, no fever, and symptoms that were present for at least two weeks, making an acute orbital cellulitis very unlikely. Other diagnostic laboratory studies include thyroid function tests, ESR, ANA, ACE, and ANCA. Orbital imaging is indicated in most cases and CT is the most common means. MRI, however, may offer advantages in distinguishing inflammation FROM neoplasia and hemorrhage. B-scan ultrasonography is useful in cases of anterior pseudotumor or posterior scleritis to evaluate choroidal effusions and may SHOW the characteristic T-sign of a sub-tenons effusion. Orbital biopsy is indicated if there is a prior history of systemic malignancy, uncertainty of the diagnosis, or in cases that are refractory to treatment.
Corticosteroids are the mainstay of treatment and the response can be impressive as seen in our case. Oral prednisone at a starting dose of 60-100 mg is used for 2-3 weeks followed by a taper. Alternative treatments for cases that are refractory to steroids and for patients who become steroid-dependent include low dose radiation, cyclosporin, methotrexate, and cyclophosphamide.
2) Benson WE. Posterior scleritis. Surv Ophthalmol 32:297 (1988).
3) Kennerdell JS, Dresner SC. The nonspecific orbital inflammatory syndromes. Surv Ophthalmol 29:93 (1984).
4) Mauriello JA, Flanagan JC. Management of orbital inflammatory disease. A protocol. Surv Ophthalmol 29:104 (1984).