77 year old woman seen in the optometry clinic for aphakic contact lenses
Digital Journal of Ophthalmology 1998
Volume 4, Number 15
February 28, 1998
Volume 4, Number 15
February 28, 1998
POHx: Bilateral intracapsular cataract extraction 25 years ago. PMMA contact lens user since 1972
PMHx: Non-Contributory
Meds: Motrin
SHx: Non-contributory
FHx: Non-contributory
External exam: Normal
Pupils: Reactive to light, no APD OU
Motility: Full OU
Slit lamp examination: See figures 1-3
Endothelial Specular Microscopy: See figures 4-6
Intraocular pressure: 14 mm Hg OD, 14 mm Hg OS
Fundi: Normal OU
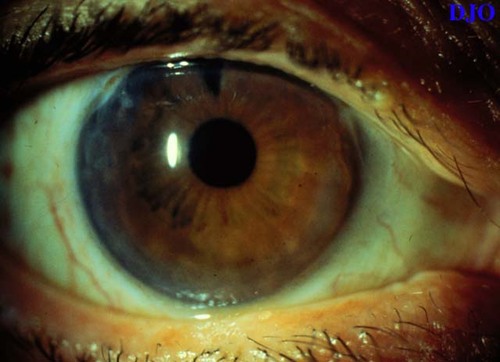
Figure 1
Figures 1-3. There is peripheral concentric corneal edema extending 2.5-3.5 mm FROM the limbus. The patient has a peripheral iridectomy and is aphakic OD. The left eye had a similar appearance.
Figures 1-3. There is peripheral concentric corneal edema extending 2.5-3.5 mm FROM the limbus. The patient has a peripheral iridectomy and is aphakic OD. The left eye had a similar appearance.

Figure 2
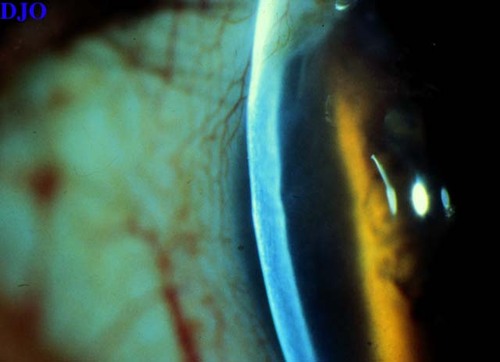
Figure 3
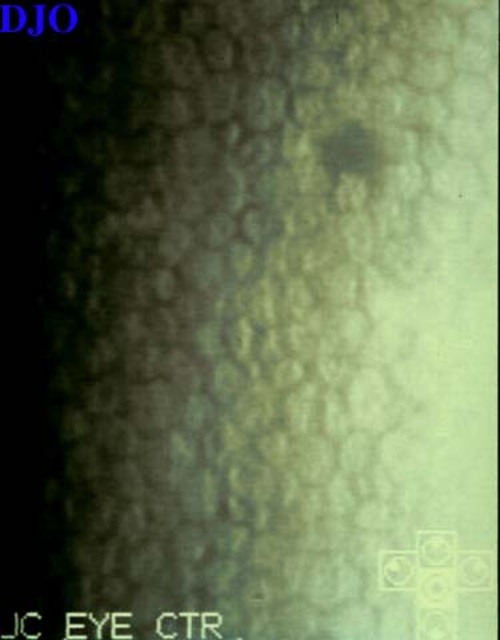
Figure 4
Figures 4-6. Specular microscopy of the center of the cornea is essentially normal(left), Specular microscopy of the peripheral cornea (center and right) shows polymegathism and decreased numbers of corneal endothelial cells
Figures 4-6. Specular microscopy of the center of the cornea is essentially normal(left), Specular microscopy of the peripheral cornea (center and right) shows polymegathism and decreased numbers of corneal endothelial cells
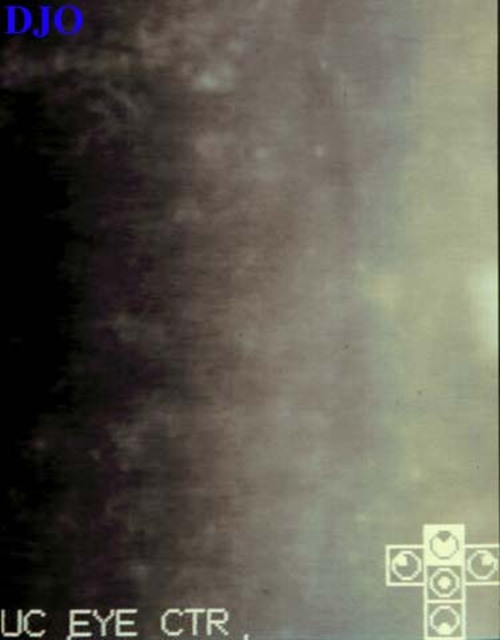
Figure 2
Figure 6
- Marginal keratopathy related to collagen vascular disease
- Fuch's endothelial dystrophy
- Endotheliitis
- Furrow degeneration
- Brown-McLean Syndrome
This is a form of peripheral corneal edema involving both stroma and epithelium without vascularization. The condition occurs long after cataract surgery and has not been seen earlier than 6 years. The syndrome was first described by Brown and McLean in 1969.
Corneal edema extends 2 to 3 mm centrally FROM the limbus for 360 degrees. The superior limbus may be clear, particularly if there is a superior sector iridectomy. In most cases, fine pigment is deposited on the endothelium in the involved areas. Endothelial cell density may be decreased, however, the central cornea rarely becomes edematous.
Atrophy of the peripheral iris may be seen by transillumination. This atrophy is probably not the result of liberation of iris pigment because the trabecular meshwork is not unduly pigmented in these cases. Although altered aqueous dynamics, iridodonesis, and movement of other tissues or the intraocular lens have been proposed as etiologies, the cause of the syndrome remains unknown.
This syndrome occurs mostly in aphakic eyes, though patients with extracapsular cataract extraction, anterior chamber lenses, as well as posterior chamber lenses have been described. The reports of involved siblings and frequent bilaterality may suggest a possible genetic predisposition. Most patients require no therapy, however, penetrating keratoplasty and peripheral conjunctival flaps have been used for pain control.
2) Jaffe NS, Jaffe MS, Jaffe GF eds. Cataract Surgery. 429 (1990)