24 year old woman with blurry vision and photophobia OS
Digital Journal of Ophthalmology 1998
Volume 4, Number 14
January 30, 1998
Volume 4, Number 14
January 30, 1998
POHx: None
PMHx:Three years prior to presentation, the patient was diagnosed with acute lymphoblastic leukemia for with she was treated with chemotherapy and radiation
Meds: Pred Forte 1% OS qid
SHx: Non-contributory
FHx: Non-contributory
External exam: Normal
Pupils: 3 --> 2 OD 4 --> 3 OS
Motility: Full OU
Slit lamp examination: Normal OD, the exam in the left eye is shown in Figure 1.
Intraocular pressure: 19 mm Hg OD, 18 mm Hg OS
Fundi: Normal OU

Figure 1
Figures 1-2. The left cornea showed diffuse endothelial dusting with debris. The anterior chamber had 2+ flare and 3-4+ cells and a hypopyon. The hypopyon was streaked with some red blood cells. The left iris appeared more white than the right, had dilated vessels and was thickened. The lens was clear.
Figures 1-2. The left cornea showed diffuse endothelial dusting with debris. The anterior chamber had 2+ flare and 3-4+ cells and a hypopyon. The hypopyon was streaked with some red blood cells. The left iris appeared more white than the right, had dilated vessels and was thickened. The lens was clear.

Figure 2
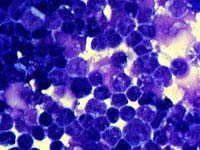
Figure 3
Because of the concern of a relapse of acute lymphoblastic leukemia (ALL), an anterior chamber paracentesis was performed to obtain cytology. High magnification revealed a malignant lymphoid cell infiltrate compatible with a recurrence of ALL
Because of the concern of a relapse of acute lymphoblastic leukemia (ALL), an anterior chamber paracentesis was performed to obtain cytology. High magnification revealed a malignant lymphoid cell infiltrate compatible with a recurrence of ALL
After the diagnosis ALL recurrence, the patient underwent bone marrow biopsy, lumbar puncture, and head MRI, none of which demonstrated any other areas of recurrence. The patient was treated with topical Pred Forte 1%, intrathecal methotrexate, and systemic daunorubicin, vincristine, and dexamethasone as well as radiation.
Background:
Acute leukemia is the most common malignancy in children. Acute lymphoblastic leukemia (ALL) is the most common variety, accounting for 70-90%, and is characterized by uncontrolled proliferation of primitive white cells (blasts) in the bone marrow.
Clinical Features:
Ophthalmic involvement in leukemia can occur in up to 90% of patients. The choroid is the most commonly involved site although this is not always clinically apparrent. Ocular and orbital involvement can manifest as skin infiltration, extraocular muscle palsies, diplopia, proptosis, subconjunctival hemorrhage, sterile ring ulcers, anterior segment necrosis, ciliary body involvement, vitreous leukemic infiltrates, retinal hemorrhages, cotton wool spots, serous retinal detachments, RPE changes, papilledema, or optic nerve infiltration. Hyperviscosity states can manifest as retinal microaneurysms, venous occlusive disease, and retinal neovascularization. Opportunistic infections are common. Complications of therapy include radiation or steroid related cataracts, radiation retinopathy, and chemotherapeutic agent side effects.
Involvement of the anterior segment is actually rare and is found in 0.5-2.5% of all leukemic relapses. Symptoms can include redness, photophobia, changes in pupil shape or color, pain, and visual loss. Clinically, anterior segment leukemic infiltrates can be distinguished FROM anterior uveitis in that leukemic involvement presents more commonly with normal or slightly decreased pupil size, segmental or total ciliary injection, segmental or diffuse iris swelling, hypopyon and hyphema, increased intraocular pressure, and rarely with posterior synechiae. Anterior uveitis tends to present with miotic pupils, total ciliary injection, flat irides, low intraocular pressures, posterior synechiae, and less commonly with hypopyon or hyphema.

Figure 4
This photograph of the left eye was taken 3 months after initiation of treatment. Note the resolution of the pseudo-hypopyon.
This photograph of the left eye was taken 3 months after initiation of treatment. Note the resolution of the pseudo-hypopyon.
2) MacLean H, Clarke MP, Strong NP, et al. Primary Ocular Relapse in Acute Lymphoblastic Leukemia. Eye. 10:719-22 (1996)
3) Rosenthal AR. Ophthalmic Manifestations of Leukemia: A Review. Ophthalmology 90:899-905 (1983)