34 year old man with a dull ache around his left eye
Digital Journal of Ophthalmology 1998
Volume 4, Number 13
January 7, 1998
Volume 4, Number 13
January 7, 1998
POHx: None
PMHx: Non-contributory
Meds: acetominophen
SHx: Non-contributory
FHx: Non-contributory
External exam: (see Figure 1)
Pupils: 3 --> 2 OD 4 --> 3 OS
Motility: Full OU
Slit lamp examination: (see Figure 2)
Intraocular pressure: 15 mm Hg OD, 45 mm Hg OS
Gonioscopy: Angles open 360 degrees OU. No synechiae present or neovascularization.
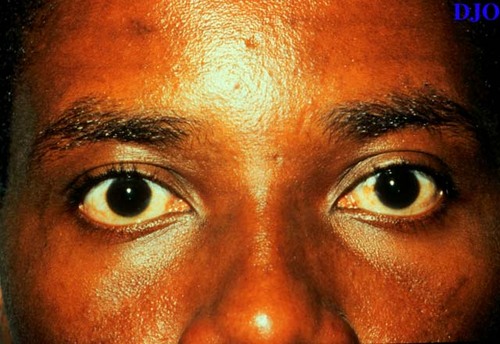
Figure 1
The patient's external features were normal. The left pupil can be seen to be slightly larger than the right pupil.
The patient's external features were normal. The left pupil can be seen to be slightly larger than the right pupil.

Figure 2
Figures 2-3. Corneas were clear bilaterally. Conjunctiva were white and quiet OU. The anterior chambers appeared deep OU. There was 1+ flare and rare cell in the anterior chamber OS. The anterior chamber OD was quiet. Irides and lenses appeared normal.
Figures 2-3. Corneas were clear bilaterally. Conjunctiva were white and quiet OU. The anterior chambers appeared deep OU. There was 1+ flare and rare cell in the anterior chamber OS. The anterior chamber OD was quiet. Irides and lenses appeared normal.
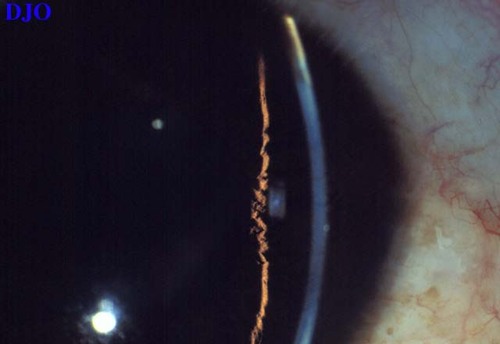
Figure 3
- Pigment dispersion glaucoma
- Posner-Schlossman's syndrome (glaumatocyclitic crisis)
- Angle recession glaucoma
Our patient was diagnosed with Posner-Schlossman's syndrome because of the small amount of inflammation in the affected eye with open angles and absence of other pathologic findings. The slightly dilated pupil in the affected eye was also characteristic of the condition.
Background:
Glaumatocyclitic crisis was first described by Posner and Schlossman in 1942. The syndrome is characterized by recurrent attacks of very mild inflammation that is associated with markedly elevated intraocular pressure. This condition usually occurs between the ages of 20 and 50 and is unilateral and recurrent.
Clinical Features:
Symptoms include mild discomfort and blurred vision and haloes if corneal edema is present. The affected eye typically appears white and quiet on gross inspection, but a small amount of inflammation can usually be detected. The anterior chamber is deep. A common finding is that the pupil is slightly dilated in the affected eye compared to the unaffected eye. Posterior and anterior synechiae do not form in this condition. Although attacks are self limited, glaucomatous cupping and field loss may occur.
Pathogenesis:
The exact etiology of this condition is unknown. However, the increased introcular pressure is associated with an acute decrease in outflow facility which resolves when the attack breaks. Elevated levels of prostaglandins in the aqueous humor have been found during acute attacks. Potentially, the increased levels of prostaglandins may be responsible for the decreased outflow facility and breakdown of the blood aqueous barrier with release of proteins and cells INTO the anterior chamber.
Treatment:
In the acute situation, topical corticosteroids are used to decrease the inflammation and topical aqueous suppressants and oral carbonic anhydrase inhibitors are useful to control the intraocular pressure. Miotics should be avoided because of the potential to increase intraocular inflammation. Given the possible role of prostaglandins in this condition, prostaglandin inhibitors such as oral indomethacin have been tried with anecdotal success.
2) Masuda K, Izawa Y, Mishima S: Prostaglandings and glaumatocyclitic crisis. Jpn J Ophthalmol 19:368 (1975)