30 year old female with recurrent left orbital mass
Digital Journal of Ophthalmology 2001
Volume 7, Number 5
September 1, 2001
Volume 7, Number 5
September 1, 2001
Past ocular history was notable for excision of a left orbital cyst at age 13. She noted swelling of the left upper lid with crying but denied tear formation.
Past Ocular History: none
Past Medical History: none
Medications: Oral contraceptives, Retin A, Cleocin, and Hydrocortisone creams
Family History: Non-contributory.
Vision: 20/20 OU
Pupils: Equal, round, and reactive to light. No afferent pupillary defect
Motility: Full OD. 3/4 abduction OS. Diplopia in left gaze only, beginning at approximately 45 degrees.
External exam: S-shaped deformity of the left upper lid with fullness of the superotemporal quadrant. Palpation revealed a soft, doughy mass in that area. There was a surgical scar just underneath the left brow with some thinning of the brow hair.
Exophthalmometry: 3 mm proptosis of the left globe.
Slit lamp exam: normal OU
Fundus exam: normal OU

Figure 1
Figures 1-2. Photographs of this patient reveal fullness of the upper, outer quadrant of the left upper eyelid, creating an S-shaped contour. There is mild ptosis and proptosis as well.
Figures 1-2. Photographs of this patient reveal fullness of the upper, outer quadrant of the left upper eyelid, creating an S-shaped contour. There is mild ptosis and proptosis as well.
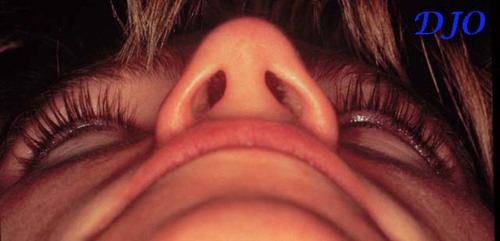
Figure 2
Pathology

Figure 3
Figures 3-5. CT scans demonstrate a cystic lesion in the upper, outer quadrant of the orbit. Axial views reveal attenuation of the lateral wall of the orbit.
Figures 3-5. CT scans demonstrate a cystic lesion in the upper, outer quadrant of the orbit. Axial views reveal attenuation of the lateral wall of the orbit.

Figure 4
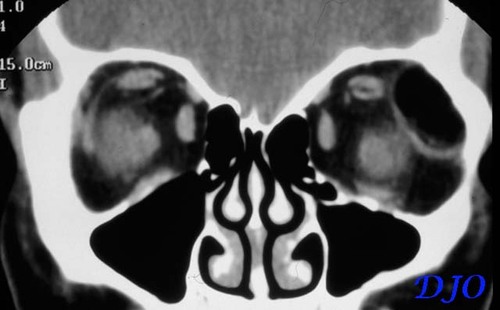
Figure 5
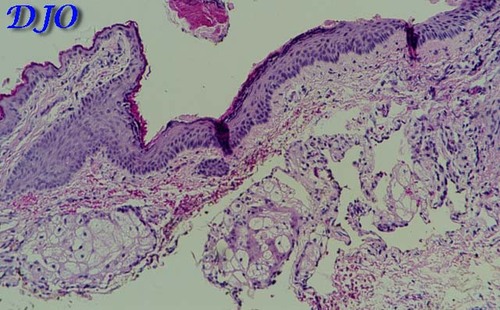
Figure 6
Figures 6-7. Histologic sections reveal the cyst wall, comprised of stratified squamous epithelium with epidermal appendages, such as the hair follicle seen in Figure 7. Also, note the inflammatory infiltrate in the surrounding tissue.
Figures 6-7. Histologic sections reveal the cyst wall, comprised of stratified squamous epithelium with epidermal appendages, such as the hair follicle seen in Figure 7. Also, note the inflammatory infiltrate in the surrounding tissue.
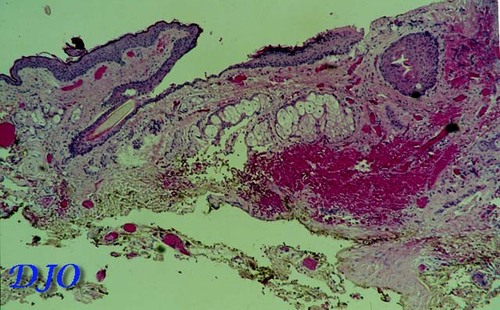
Figure 7
- cholesterol granuloma
- mucocele
- aneurysmal bone cyst
- lipodermoid
- malignant neoplasm, e.g. squamous cell or adenocarcinoma
- idiopathic inflammatory pseudotumor
- lymphoid tumor
- epithelial tumor of lacrimal gland
Dermoid cysts are congenital tumors which are thought to arise FROM areas of ectoderm pinched off along bone suture lines. They comprise approximately 3-9% of all orbital masses and are the most common orbital tumors in children. It has been reported that 10-50% of dermoids occurring in the head and neck region are orbital. The superotemporal quadrant is the most common location with the frontozygomatic suture as a frequent site of attachment. Histologically, these tumors are composed of a wall of stratified squamous epithelium with appendages such as sebaceous glands and hair follicles surrounding a keratin containing cavity. The wall of an epidermoid cysts does not contain appendages.
Dermoids typically present during childhood, but can present at any age. It has been observed that those presenting later in life are often deeper in origin and more challenging in terms of management. Superficial dermoids most often present as an asymptomatic, mobile mass. Deeper tumors may cause diplopia and proptosis. Orbital inflammation FROM leakage of cyst contents or cyst rupture following blunt trauma can also be a presenting sign.
CT scan is extremely valuable in establishing the diagnosis of dermoid tumors. They characteristically appear cystic and arise in close relationship to bone. Often there are abnormalities of the adjacent bone. Tumors may create a fossa in the underlying bone or erode through the bone INTO the temporal fossa ("dumbbell" tumor) or rarely the intracranial space. In a recent study, Sathananthan, et al. reviewed CT scans of 70 patients with outer canthus dermoid cysts and identified several types of bony abnormalities which they classified as pressure erosion, abnormal shape, tunnel or canal, pit or crater, cleft, and abnormal texture. They identified pressure erosion in 87% of their series and an abnormal shape thought not secondary to pressure erosion in 79%. Dermoids were both intra- and extraorbital in 43% of the cases reviewed, with extension INTO the temporal fossa in the majority of these cases. They suggest that the presence of dermoid cysts may lead to developmental anomalies in the surrounding bone.
Clinically, the presence of bony changes may support the diagnosis of dermoid, but should also bring INTO consideration malignant tumors of the orbit which may erode bone. Additionally, knowledge of bone involvement may influence surgical management. The goal of treatment is complete excision on the first attempt. Excision is achieved via anterior and/or lateral orbitotomy. A common cause of recurrence is residual tumor within bone. Therefore, drilling of tunnels or clefts in involved bone should accompany careful dissection of the entire cyst wall. Removal of a segment of the lateral orbital bone is sometimes necessary to achieve adequate exposure. In those cases where complete excision in impossible, some have advocated marsupialization. However, others such as Sherman, et al. point to the risk of infection and recommend against it.
The patient presented here underwent lateral orbitotomy and the recurrent dermoid was successfully excised. Dissection of the cyst proved to be challenging because of obliteration of tissue planes as a result of chronic inflammation and previous surgery. There was significant thinning and a very small tunnel in the area of the lateral orbital bone which appeared abnormal on CT scan. This area was drilled during the procedure in ORDER to remove all remnants of the cyst wall.
On pathology, there was histologic evidence of inflammation in the tissues surrounding the cyst, suggestive of leakage. This inflammation could account for the painful, throbbing sensation experienced by the patient. Lane , et al. examined a series of 40 cases of orbital dermoid cysts and found that of the seven patients who had complained of pain or tenderness, all had evidence of chronic inflammation on histology. Two patients in this series who had had previous incomplete excision of dermoid cysts had chronic inflammation resulting in fistula formation with drainage throught the conjunctiva in one case and through the skin in the other.
Leonardo, et al. dsecribe a case of an infant with a giant orbital dermoid cyst, all of which was excised intially except for a small remnant tightly adherent to the structures of the orbital apex. Nine months after the surgery, fullness of the lateral canthal area and persistent conjunctival chemosis was noted. Radiologic studies revealed a recurrent cystic lesion and a second lateral orbitotomy revealed "a disorganized dermoid cyst surrounded by extensive fibrotic connective tissue" which required a "lengthy, meticulous dissection." Thus, it is important to emphasize that incomplete excision of a dermoid cyst can not only lead to recurrence months to years later, but can also be complicated by consequences of chronic inflammation such as fibrosis and fistula formation. In such circumstances, excision can be challenging as well as tedious.
2) Lane, C.M., Ehrlich W.W., and Wright J.E. Orbital dermoid cyst. Eye, 1: 504 (1987)
3) Leonardo, D.O., Shields C.L., Shields J.A., and Nelson, L.B. Recurrent giant orbital dermoid of infancy. J Pediatr Ophthalmol Stabismus, 31: 50 (1994)
4) Sathananthan, N., Moseley, I.F., Rose, G.E., and Wright, J.E. The frequency and clinical significance of bone involvement in outer canthus dermoid cysts. Br J Ophthalmol, 77: 789 (1993)
5) Sherman, R.P., Rootman, J., and Lapointe, J.S. Orbital dermoids: clinical presentation and management. Br J Ophthalmol, 68: 642 (1984)