39 year old male with diplopia on right gaze
Digital Journal of Ophthalmology 2001
Volume 7, Number 6
October 1, 2001
Volume 7, Number 6
October 1, 2001
Previous ocular history: Recurrent episodes of iritis OS beginning 6 years ago. No childhood strabismus.
No family history of ocular problems including strabismus.
Past Medical History: ankylosing spondylitis, hypertension
Medications: none
Family History: Non-contributory.
Titmus stereopsis: 40 seconds arc
Prism covertest measurements:
Distance
| X6 Prism diopters RH2 Prism diopters | ||
| (R.Gaze) XT35 PrismD RHT12 PrismD | orthophoria | orthophoria (L.Gaze) |
| Head tilt right: XT 4 PrismD RHT 2 PrismD | orthophoria | Head tilt left: X8 PrismD |
Near X'10 PrismD
Ocular rotations: Limitation in adduction OS, worse in upgaze. Globe retraction and mild down-shoot OS on attempted adduction. Normal adducting saccades (Figure 1).
View FROM Left Side: Side gaze photos demonstrating narrowing of the palpebral fissures and globe retraction OS on gaze right (Figure 2).
Hertel expophthalmometry: Base 102 mm, OD 19 mm, OS 20 mm
Slit lamp exam: OD normal; OS old iris pigment adhesions on anterior lens capsule, anterior chamber clear and quiet, no cells or flare.
Fundus: Unremarkable OD & OS
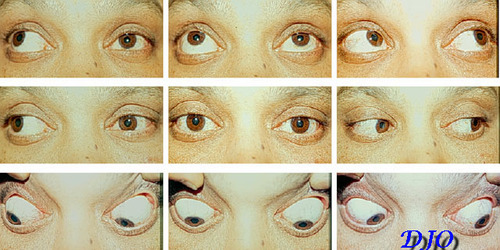
Figure 1
Ocular Rotations
Ocular Rotations

Figure 2
Side View
Side View

Figure 3
one month Post-op
one month Post-op
The patient was insistent that this was an acquired condition, not congenital. A CT scan of the head and orbits was carried out:
Orbits - no evidence of mass or other lesion. extraocular muscles: normal.
Head - subarachnoid space and ventricles, brain stem and posterior fossa: normal.
- Acquired pseudo-type II Duane's syndrome
- Orbital mass lesion OS
- Atypical thyroid orbitopathy
- Left internuclear ophthalmoplegia
- Left medial rectus palsy
The finding of globe retraction on attempted adduction and grossly normal looking adducting saccades indicated a restrictive etiology rather than a left medial rectus paresis or left internuclear ophthalmoplegia. The orbital CT scan effectively ruled out thyroid orbitopathy or orbital mass. On a subsequent visit, the patient insisted that this was acquired in the past few years and definitely not congenital. He denied any previous operations or trauma to the left eye. It was not until he was getting ready to leave that his wife asked if his ocular motility problems could be related to injections "into the eye" that he had received 5 years earlier while being treated for iritis OS. His previous ophthalmologist had since left town; however, we were able to obtain his records. These indicated that he had received a series of subconjunctival methylprednisolone injections OS under retrobulbar anaesthesia with xylocaine for iritis.
A forced duction test confirmed restriction to adduction OS and the patient was scheduled for surgery to explore the left lateral rectus. Under general anaesthesia significant scarring and fibrosis of the anterior portion of the left lateral rectus muscle was found. The left lateral rectus was recessed 5 mm to allow better adduction. This was balanced with a left medial rectus recession of 6 mm on an adjustable suture. The lateral conjunctiva was also recessed 10 mm. No post-op adjustment was required.
One month post-op:
Adduction OS was greatly improved. Patient was no longer aware of diplopia except on extreme right gaze and had no diplopia in any other field of gaze.
Prism cover test:
Distance
| orthophoria | ||
| (R.Gaze) X(XT)12 PrismD | orthophoria | E 4 PrismD (L. Gaze) |
| orthophoria |
Near X' 10 PrismD
Discussion:
Duane's Syndrome is a congenital condition caused by co-contracture of the ipsilateral lateral rectus muscle on attempted adduction. Pseudo-Duane's syndrome is a restrictive condition caused by a restrictive orbital adhesion to the globe or by tethering of the globe FROM a tight rectus muscle(1). This patient was found to have scarring and tightness of the left lateral rectus muscle producing an exotropia with globe retraction on attempted adduction. This was likely caused by inadvertent injection of Xylocaine or methylprednisolone INTO the lateral rectus muscle.
Extraocular muscle restriction secondary to local anaesthetic myotoxicity is becoming a well-recognized phenomenon. Aminoacyl local anaesthetic preparations such as Xylocaine ( lidocaine + epinephrine) and Marcaine (bupivocaine) induce necrosis when directly injected INTO muscle tissue(2). Compounds of this class have been used to induce muscle necrosis in animal and human muscle regeneration studies since the 1970's. They appear to have their effect by raising intracellular calcium levels and promoting enzyme mediated cellular breakdown (3).
Many papers have appeared in the literature over the past 10 years documenting the effects of local anaesthetic myotoxicity in humans after retrobulbar and peribulbar anaesthesia. The muscle undergoes a rapid cellular degeneration and regeneration and some patients then go on to develop fibrosis and contracture of the affected muscle and restrictive strabismus4. This appears to occur most frequently with multiple injections and higher injection volumes(5) in elderly patients (age 60-80 years) (4). The association with older patients may simply reflect the majority age range of patients receiving retrobulbar and peribulbar anaesthesia for cataract surgery.
We could find no papers in the literature linking methylprednisolone to muscle toxicity or muscle fibrosis although it is possible that the lateral rectus scarring seen in our patient was caused by direct mechanical trauma FROM a subconjunctival methylprednisolone injection and not the retrobulbar injection of Xylocaine.
2) Carlson B.M. et al., Extraocular muscle regeneration in primates: local anaesthetic induced lesions. Ophthalmology, 99:582 (1992)
3) Porter, J.D. et al., Extraocular myotoxicity of the retrobulbar anaesthetic bupivocaine hydrochloride. Invest Ophthalmol Vis Sci, 29:163 (1988)
4) Capo, H. and Guyton, D.L., Ipsilateral hypotropia after cataract surgery, Ophthalmology, 103:721 (1996)
5) Hamilton, R.C., Gimbel, H.V. and Strunin, L., Regional anaesthesia for 12,000 cataract extraction and intraocular lens implantation procedures. Can J Anaesth, 35:615 (1988)