25 year old woman with loss of vision of the left eye
Digital Journal of Ophthalmology 2001
Volume 7, Number 8
December 1, 2001
Volume 7, Number 8
December 1, 2001
PMHx: Non-contributory
Meds: None
SHx: Non contributory
FHx: Non contributory
Amsler grid: defective on upper left field
Pupils: Equal, reactive, No APD
Motility: Full OU
Visual Field: Defective on central and upper field
External: No lid swelling or conjunctival chemosis or injection.
Intraocular pressure: Normal
Slit lamp examination: Normal anterior segments
Dilated fundus examination: Normal OD
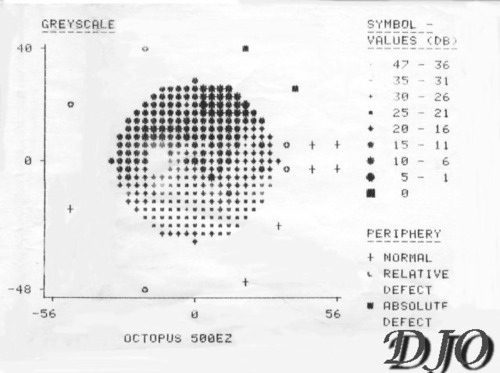
Figure 1a
G1 programme
Figures 1a-1b. Defective on central and upper field
G1 programme
Figures 1a-1b. Defective on central and upper field
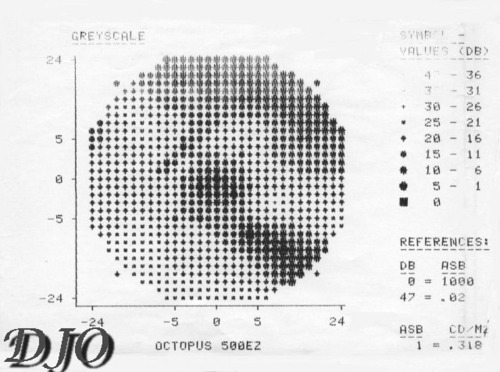
Figure 1b
M1-macula programme
M1-macula programme
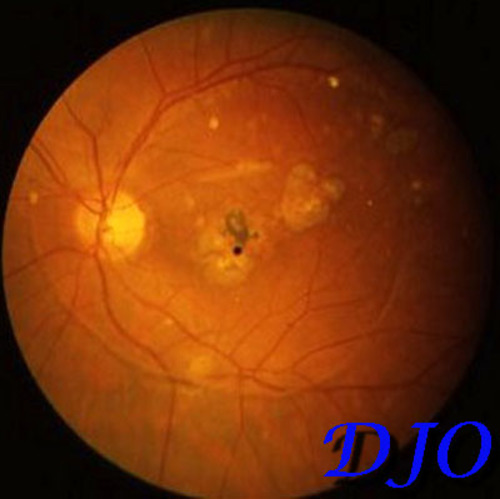
Figure 2
Hypopigmented atrophic scars and annular posterior vitreus detachment OS
Hypopigmented atrophic scars and annular posterior vitreus detachment OS
Toxoplasmosis IgM -; IgG+
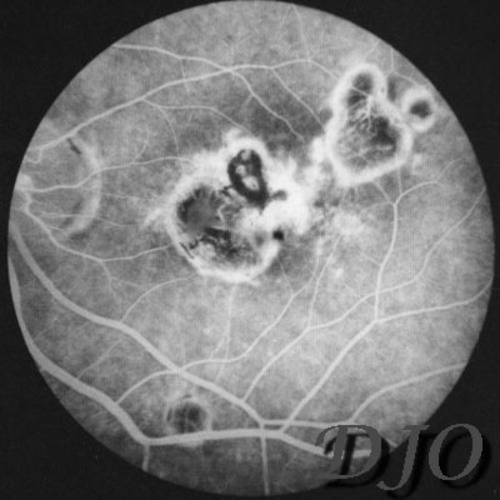
Figure 3a
Figures 3a-3b, Florescein angiogram (OS). Fluorescein angiogram showing areas of hyperfluorescence (a) which increases at the late phase(b); window defects as well as atrophic scars on the left macular region are seen.
Figures 3a-3b, Florescein angiogram (OS). Fluorescein angiogram showing areas of hyperfluorescence (a) which increases at the late phase(b); window defects as well as atrophic scars on the left macular region are seen.
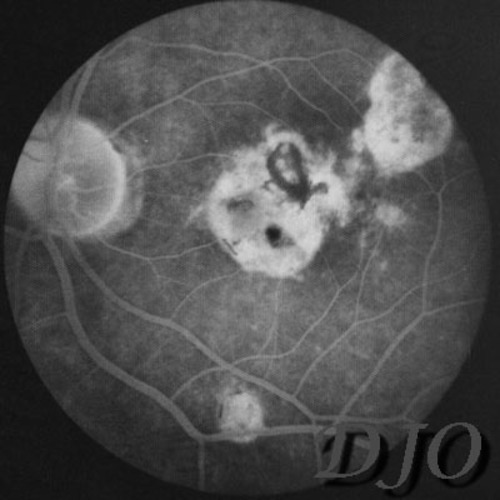
Figure 3b
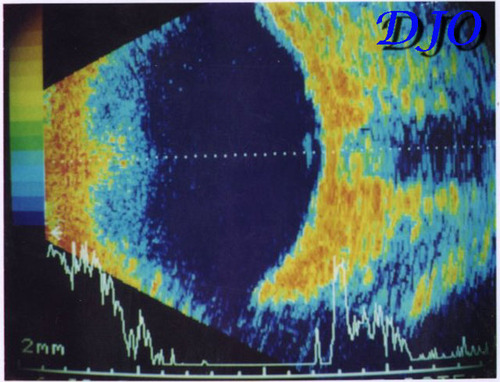
Figure 4
Ultrasonography (OS). PVD is seen as a vertical line at the posterior fundus.
Ultrasonography (OS). PVD is seen as a vertical line at the posterior fundus.
- normal aging
- PVD caused by proliferative diabetic retinopathy
The patient was diagnosed as HAVING PVD caused by toxoplasma retinitis; she was followed up regularly and conservatively without treatment. The visual symptoms as well as the ophthalmic findings remained the same during a follow-up period of 2 years.
Posterior vitreous detachment (PVD) is the separation of the vitreous base FROM the adjacent retina. During embryonic and early postnatal development the vitreous cavity is totally filled with gel vitreous. With subsequent growth of the eyeball the relative volume of liquid vitreous increases progressively, the resultant lacunae coalesce and form progressively larger cavities of liquid vitreous, resulting in PVD. There appears to be a linear relationship between vitreous liquefaction and PVD and the prevalence of PVD increases dramatically after 50 percent liquefaction is reached. The precipitating factors for for PVD is not clear. A series of progressive changes, starting with vitreous liquefaction and shrinkage of the fibrous component of the vitreous, especially the posterior cortical layer is believed to play an important role. Shrinkage of the posterior cortical fibers may cause the posterior cortex to contract anteriorly. These changes may also weaken the attachment of the cortex to the retina. Sudden movements of the eyeball or gravitational forces may trigger the occurrence of PVD. As the posterior vitreous cortex retracts FROM the posterior pole, liquefied vitreous can rush through defects in the posterior cortex. The precipitating event may be a tear in the posterior cortical vitreous in the region of the macula; fluid FROM the central part of the liquefied vitreous can pass through a break in the vitreous cortex and separate the surrounding cortical vitreous FROM the retina (1).
Kakehashi et al (2) classified PVD variations INTO four types; complete PVD with collapse (age-related type or myopia associated), complete PVD without collapse (uveitis and CRVO associated ), partial PVD with thickened posterior vitreous cortex (proliferative diabetic retinopathy), or partial PVD without thickened posterior vitreous cortex (patients without retinal disease). The factors associated with PVD are vitreous liquefaction, vitreous shrinkage and weakening of vitreoretinal adhesion. Vitreous liquefaction is frequently associated with aging or in eyes with degenerative myopia.
Typical symptoms of vitreous detachment are light flashes, showers in the field of vision An annular opacity is seen ophthalmoscopically (Fig 2) , which represents the hyaloid attachment to the optic nerve. PVD can be mistaken with syneresis. PVD plays a significant role in retinal detachment since it may precipitate retinal breaks. Horseshoe tear is one of the most dangerous types of retinal break, because the vitreous usually remains adherent to the flap of the tear, still exerting continuous traction. On the other hand, round breaks with free-floating opercula are less dangerous since a plug of retina has been pulled completely free FROM its surroundings by the contracting vitreous, as in our case . Age is the most common cause of PVD. Diabetes, inflammation, and extraretinal hemorrhages are less common predisposing disorders. In the first and second decades of life, retinitis pigmentosa, nondiabetic retinal vascular disorders, and a history of ocular contusion were most commonly associated with PVD. In the third decade, proliferative diabetic retinopathy was the condition most commonly associated with PVD (3). Inflammatory diseases of various aetiology produce opacification, liquefaction, and shrinkage. Additional changes include cellular proliferation and transformation leading to fibrosis in cases of prolonged inflammation. In some eyes the fibrosis is primarily cortical while in others it is extensive (4).Many Many mm intraocular inflammatory and infectious conditions can cause vitreous gel liquefaction , PVD and retinal breaks. Ocular toxoplasmosis, toxocariasis and pars planitis are examples which may be associated with vitreoretinal changes causing retinal breaks.
Bodanowitz and his co-workers reported retinal tear in retinitis associated with toxoplasmosis (5). Retinal tears or rhegmatogenous retinal detachment are rare complications of toxoplasmic retinochoroiditis. However, a tear may occur due to vitreoretinal traction following postinflammatory structural alteration of the vitreous.
The vitreous of 39 eyes with ocular toxoplasmosis was studied and photographed using an El Bayadi-Kajiura preset lens. In active cases of toxoplasmosis, the vitreous showed inflammatory opacities and gel shrinkage. In inactive cases, the vitreous was often liquefied. Compared with 39 normal eyes of age- and sex-matched controls, the prevalence of partial PVD was significantly higher in toxoplasmosis. A higher prevalence of PVD was found in eyes with the major chorioretinal lesion outside the temporal vascular arcade than in those with lesions inside the temporal vascular arcade. (6).
In patients with PVD, vitreous structure must be thoroughly examined and structural changes in the retina assessed carefully to reveal the underlying pathology.
2) Kakehashi, A.; Kado, M.; Akiba, J.; Hirokawa, H. Variations of posterior vitreous detachment. Br J Ophthalmol, 81:527-532 (1997)
3) Hikichi, T.; Trempe, C.L . Ocular conditions associated with posterior vitreous detachment in young patients. Ophthalmic Surg Lasers, 27: 782-6 (1996)
4) Hogan, M.J. Inflammation and its effect on the vitreous. Trans Ophthalmol Soc UK, 95: 378-81 (1975)
5) Bodanowitz, S.; Hesse, L.; Schroeder, B. Retinal tear in retinochoroiditis toxoplasmotica. Klin Monatsbl Augenheilkd, 208: 130-1 (1996)
6) Hirokawa, H.; Trempe, C.L.; Takahashi, M.; Kado, M.; Akiba, J.; Yoshida, A.Biomicroscopic evaluation and photography of ocular toxoplasmosis. Ann Ophthalmol, 21: 379-83 (1989)