A 26-year-old man with ocular complications after adverse reaction to phenytoin
Digital Journal of Ophthalmology 2016
Volume 22, Number 4
October 4, 2016
DOI: 10.5693/djo.03.2015.05.002
Volume 22, Number 4
October 4, 2016
DOI: 10.5693/djo.03.2015.05.002
Download PDF

Figure 1
Epidermal sloughing and hemorrhagic crusting of oral mucosa.
Epidermal sloughing and hemorrhagic crusting of oral mucosa.
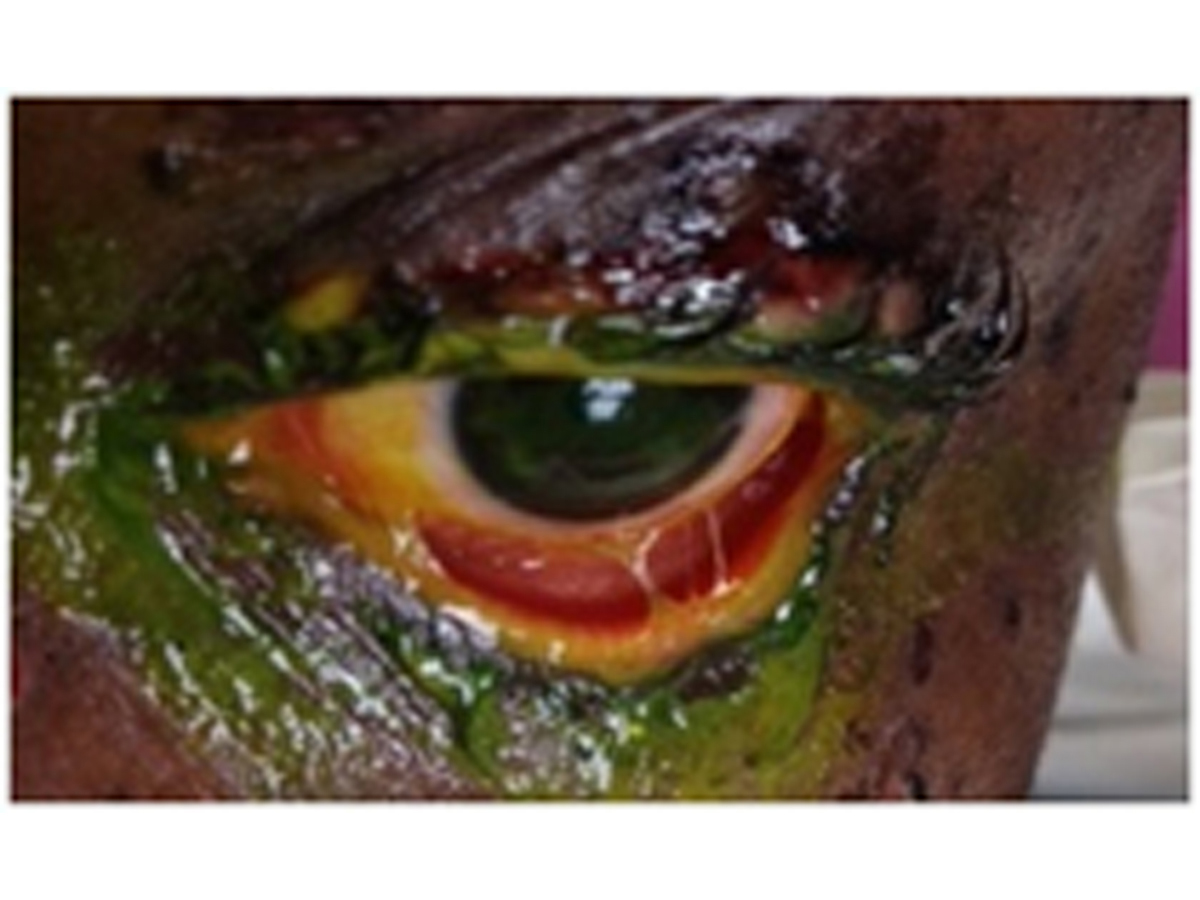
Figure 2
Presence of symblephara and significant conjunctival hyperemia.
Presence of symblephara and significant conjunctival hyperemia.
The patient was followed closely for complete resolution of ocular surface damage and continued to remain asymptomatic of long-term sequelae at the 3 months’ follow-up, with a visual acuity of 20/30 in each eye at last follow-up.(3)
Staphylococcal scalded skin syndrome is caused by an exfoliative toxin produced by roughly 5% of Staphylococcus aureus. These toxins can lead to a red rash and separation of the epidermis with diffuse sheetlike desquamation.
Toxic shock syndrome is a potentially fatal illness caused by enterotoxin type B produced by Staphylococcus aureus. Patients demonstrate presence of an infection and systemic symptoms.
Phototoxic skin reaction refers to the development of cutaneous disease as a result of the combined effects of a chemical and light. Typically, they appear as an exaggerated sunburn response, but only on sun-exposed areas of the body.
Numerous other conditions may present in a similar fashion, including trachoma, cicatricial conjunctivitis secondary to chronic topical medications (especially pilocarpine, phospholine iodide and antiviral agents), chemical burn, and radiation treatment. In addition to the entities mentioned above, the possibility of a malignant process (eg, conjunctival intraepithelial neoplasia and squamous cell carcinoma) should always be considered, particularly in older patients with risk factors.
Incidence of ocular involvement during the acute phase is between 50% and 88%(4,6) and chronic complications have been noted in up to 35% of survivors.(2) An inflammatory reaction involving the ocular surface destroys goblet cells and results in decreased secretion of mucin, which impairs tear distribution and stability. Frank scarring of the bulbar and forniceal conjunctivae can lead to symblepharon or ankyloblepharon, which cause inadequate blinking/closure and affect ocular motility. Loss of the normal glandular structures of the ocular surface and eyelids leads to severe dry eye problems and vision loss.(2)
The optimal acute ocular therapeutic regimen for TEN remains a topic for continued debate. Various interventions have been proposed, including intravenous methylprednisolone, topical steroids, and immunomodulator as well as a “Triple TEN” acute ocular management protocol, which comprises administration of triamcinolone into each of the fornices, insertion of a scleral shell spacer, and placement of amniotic membrane tissue over the corneal and limbal regions.(7)
2. Chang YS, Huang FC, Tseng SH, Hsu CK, Ho CL, Sheu HM. Erythema multiforme, Stevens-Johnson syndrome, and toxic epidermal necrolysis: acute ocular manifestations, causes, and management. Cornea 2007;26:123-9.
3. De Rojas MV, Dart JKG, Saw VPJ. The natural history of Stevens Johnson syndrome: patterns of chronic ocular disease and the role of systemic immunosuppressive therapy. Br J Ophthalmol 91;2007:1048-53.
4. Morales ME, Purdue GF, Verity SM, Arnoldo BD, Blomquist PH. Ophthalmic manifestations of Stevens-Johnson syndrome and toxic epidermal necrolysis and relation to SCORTEN. Am J Ophthalmol 2010;150:505-10.e1.
5. Fu Y, Gregory DG, Sippel KC, Bouchard CS, Tseng SCG. The ophthalmologist’s role in the management of acute Stevens-Johnson syndrome and toxic epidermal necrolysis. Ocul Surf 2010;8:193-203.
6. Sotozono C, Ueta M, Koizumi N, et al. Diagnosis and treatment of Stevens-Johnson syndrome and toxic epidermal necrolysis with ocular complications. Ophthalmology 2009;116:685-90.
7. Tomlins PJ, Parulekar MV, Rauz S. “Triple-TEN” in the treatment of acute ocular complications from toxic epidermal necrolysis. Cornea 2013;32:365-9.