A 45-year-old man with spontaneous hyphema of the right eye
Digital Journal of Ophthalmology 2017
Volume 23, Number 3
August 9, 2017
DOI: 10.5693/djo.03.2017.02.003
Volume 23, Number 3
August 9, 2017
DOI: 10.5693/djo.03.2017.02.003
Download PDF
The current episode started 1 week prior to presentation with pain, redness, and right eye photosensitivity. He was examined by his ophthalmologist 3 days later and was started on topical prednisolone acetate 1% every 2 hours. His symptoms did not improve with this treatment, and 1 day prior to presentation he was noted by his ophthalmologist to have a new hyphema of the right eye and was referred to our institution.
The patient did endorse a history of intermittent joint pains, worse in the morning but improving with movement. He had a history of back surgery 20 years prior for a herniated disc. He otherwise denied a history of autoimmune disease, fever or chills, joint pains, rashes, muscle aches, or oral ulcers. He denied a history of trauma, use of blood thinners, history of bleeding disorders, or sickle cell disease. His past medical history was unremarkable, and he did not have a history of diabetes. He did not take any medications. His family history was significant for his mother having rheumatoid arthritis.
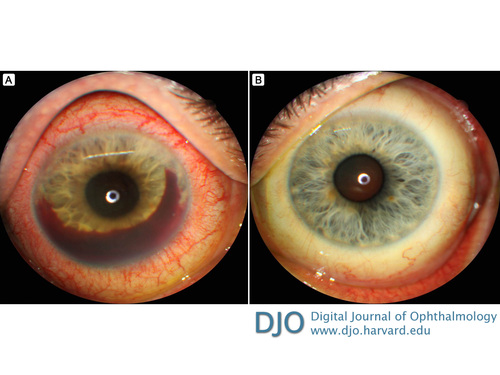
Figure 1
Anterior segment photographs of the right eye (A) and the left eye (B).
Anterior segment photographs of the right eye (A) and the left eye (B).
Fuchs heterochormic iridocyclitis was initially considered, given the presence of fine keratic precipitates and what appeared to be fine blood vessels traversing the angle. There was also an asymmetry in the color of the iris, although the iris was darker in the affected eye. A hyphema can occur due to bleeding of fine vessels traversing the iris and angle during anterior chamber paracentesis, or even spontaneously, also known as Amsler’s sign. However, the anterior uveitis in Fuchs is typically mild and rarely presents with visual acuity worse than 20/40.(1)
In our patient, the anterior chamber inflammation was quite significant and could not be adequately controlled with topical difluprednate. Due to the possibility of a viral infection, the patient was empirically started on oral antiviral therapy. It was important to obtain a sample of the aqueous humor to rule out a viral infection with PCR tests for herpes simplex and varicella zoster virus, because these have been implicated in keratouveitis and spontaneous hyphema.(2,3) In children, juvenile xanthogranulomatosis and juvenile idiopathic arthritis can also present with uveitis and spontaneous hyphema, but our patient is out of this age group.(4,5) Lens-induced uveitis and hyphema with resolution upon cataract extraction has been reported, but there was not a significant cataract in our patient.(6)
Labwork revealed our patient to be HLA-B27 positive. The uveitis associated with HLA-B27 is typically unilateral and can be severe. Spontaneous hyphema has been reported, especially in patients with ankylosing spondylitis.(3,7) It is thought that hyphema occurs in the setting of severe anterior uveitis secondary to breakdown of the blood–aqueous barrier and increase in capillary permeability.(8) Our patient did not carry a diagnosis of ankylosing spondylitis, although he did have a history of intermittent mild joint pains, improving with movement. It is not known whether recent spinal imaging has been performed to evaluate for this, but it should be considered.
Our patient’s uveitis was severe and could not be controlled with topical steroids. He required systemic corticosteroids in the acute phase and additional long-term steroid sparing therapy with methotrexate and adalimumab. Recent studies have shown anti-TNF-α agents such as infliximab, adalimumab, and etanercept to be effective in the treatment of uveitis associated with HLA-B27.(9,10) However, these agents increase the risk of severe infection and should be used with caution. Coordination with a rheumatologist can be helpful in the management of these patients.
2. Okunuki Y, Sakai J, Kezuka T, Goto H. A case of herpes zoster uveitis with severe hyphema. BMC Ophthalmol 2014;14:74.
3. Fong DS, Raizman MB. Spontaneous hyphema associated with anterior uveitis. Br J Ophthalmol 1993;77:635-8.
4. Shimada Y, Horiguchi M, Okubo T. Bilateral spontaneous hyphema with uveitis in a young girl. J Pediatr Ophthalmol Strabismus 41:114-5.
5. Longmuir S, Dumitrescu A, Kwon Y, Boldt HC, Hong S. Juvenile xanthogranulomatosis with bilateral and multifocal ocular lesions of the iris, cornealscleral limbus, and choroid. J AAPOS 2011;15:598-600.
6. Rathinam SR, Cunningham ET. Spontaneous hyphaema and acute ocular hypertension associated with severe lens-induced uveitis. Eye (Lond) 2010;24:1822-4.
7. Jones NP. Spontaneous hyphema associated with anterior uveitis. Br J Ophthalmol 1994;78:420.
8. Pathanapitoon K, Dodds EM, Cunningham ET, Rothova A. Clinical spectrum of HLA-B27-associated ocular inflammation. Ocul Immunol Inflamm 2016:1-8.
9. El-Shabrawi Y, Hermann J. Anti-tumor necrosis factor-alpha therapy with infliximab as an alternative to corticosteroids in the treatment of human leukocyte antigen B27-associated acute anterior uveitis. Ophthalmology 2002;109:2342-6.
10. Kim M, Won J-Y, Choi SY, Ju JH, Park YH. Anti-TNF? treatment for HLA-B27 positive ankylosing spondylitis-related uveitis. Am J Ophthalmol 2016;0:1103-8.