79 year old female with redness and swelling of the left eyelids
Digital Journal of Ophthalmology 2002
Volume 8, Number 3
March 1, 2002
Volume 8, Number 3
March 1, 2002
Past ocular history: non-contributory
Past medical history: medically controlled hypertension
no history of diabetes or allergies
mastectomy 17 years prior for carcinoma
appendectomy and hysterectomy 27 years prior
Meds: Briserin (i.e. Reserpin and Clopamid)
Pupils: Normal (OU), no APD
Motility: OD ortho, full; OS ortho; restriction on upwards gaze and downwards gaze with slight pain on eye movement in extreme upwards gaze
External:
Hertel exophthalmometry: OS 4 mm proptosis (OD 13 mm, OS 17 mm)
Slit lamp examination:
OD: 1-2+ cortico-nuclear cataracts
OS: chemosis, 1-2+ cortico-nuclear cataracts, otherwise normal
Tonometry: OD 12 mmHg, OS 13 mmHg
Fundus examination:
OD/OS within normal limits

Figure 1
External photograph of the patient
External photograph of the patient
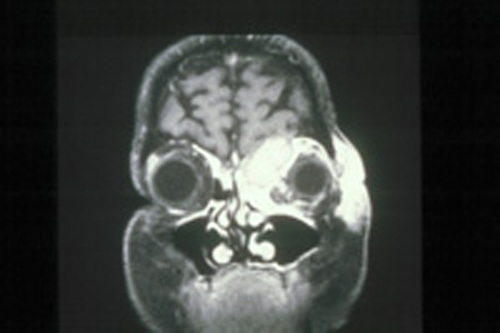
Figure 2
Figures 2-4. Ultrasound: FROM 8 to 12 o'clock in anterior and median orbit a hypodense structure could be located outside of the muscle conus. The structure
appeared regular, heterogeneous and reflectivity was low. The lesion measured approximately 14 x 19 mm and no vascularity was detected. The optic nerve and rest of the orbit appeared normal.
Figures 2-4. Ultrasound: FROM 8 to 12 o'clock in anterior and median orbit a hypodense structure could be located outside of the muscle conus. The structure
appeared regular, heterogeneous and reflectivity was low. The lesion measured approximately 14 x 19 mm and no vascularity was detected. The optic nerve and rest of the orbit appeared normal.

Figure 3
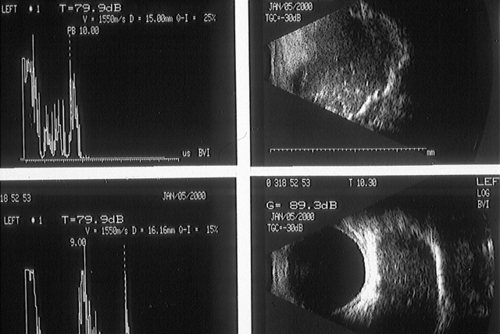
Figure 4
1) orbital abscess / cellulitis
2) orbital metastasis
Ultrasonographic differential also includes:
3) pseudo-tumor
4) lymphoma
5) sarcoma
Clinical Course:
The patient was operated on the same day by ENT service as the orbital abscess originated FROM the frontal sinus. The abscess was drained, the i.v. antibiotics were continued.
Four days later the patient was seen as follow-up. Motility was full OU, only slight pain and slight swelling were present. On Hertel no proptosis was measured.
Discussion:
Orbital cellulitis results secondarily FROM acute or chronic bacterial sinusitis in more than 90% of cases. CT scanning to evaluate the paranasal sinuses therefore is essential. Causes of orbital cellulitis include extension FROM periorbital structures (paranasal sinuses, face and eyelids, dacryocystitis, dental infection, intracranial), exogenous causes (trauma, postsurgical), endogenous septic embolization and intraorbital causes (endophthalmitis, dacryoadenitis) (1).
Antibiotics should provide coverage to multiple organisms such as gram-positive cocci, H influenzae, and anaerobes. Abscess formation is not infrequently seen and should usually be drained surgically.
In the presented case two exceptional features were encountered:
1) a very benign clinical presentation of a relatively large orbital abscess
2) difficulty of ultrasonic diagnosis of the abscess
A wide spectrum of clinical presentation of orbital abscesses exist (2), depending on localization, species of bacteria, and immune response of the patient. Age of the patient seems to be an important factor (3), with subperiostal abscesses of younger children more often clearing without drainage. Therapeutic regimens therefore have to depend on the clinical situation (4). Surgical drainage is not always necessary.
Ultrasound and CT are the two main diagnostic studies for imaging an orbita abscess. Orbital complications of inflammatory paranasal sinus diseases can be correctly diagnosed by ultrasound alone in 80 to 100% of the cases (5). Several studies indicate the high specifity and sensitivity of ultrasound diagnosis, especially when differentiating between orbital cellulitis and subperiosteal abscess (6) or when differentiating between cellulitis and pseudotumor (7). However, for localization of orbital abscesses the CT still remains the vital imaging study (7), especially when localizing the sinusitis causing the abscess. Therefore both imaging studies - CT and ultrasound - should be applied to patients, when an orbital abscess is suspected.

Figure 5
(2) Schramm VL Jr, Curtin HD, Kennerdell JS. Evaluation of orbital cellulitis and results of treatment. Laryngoscope, 1982, 92 (7): 732-8.
(3) Harris GJ. Subperiosteal abscess of the orbit: age as a factor in the bacteriology and response to treatment. Ophthalmology, 1994, 101 (3): 585-95.
(4) Hornblass A, Herschorn BJ, Stern K, Grimes C. Orbital abscess. Surv Ophthalmol, 1984, 29 (3): 169-78.
(5) Rochels R. Echographic diagnosis in orbital complications of inflammatory diseases of the paranasal sinuses. Laryngol Rhinol Otol (Stuttg), 1987, 66 (10):536-8.
(6) Kaplan DM, Briscoe D, Gatot A, Niv A, Leiberman A, Fliss DM. The use of standardized orbital ultrasound in the diagnosis of sinus induced infections of the orbit in children: a preliminary report. Int J Pediatr Otorhinolaryngol, 1999, 48 (2):155-62.
(7) Harr DL, Quencer RM, Abrams GW. Computed tomography and ultrasound in the evaluation of orbital infection and pseudotumor. Radiology, 1982, 142 (2);395-401.