A 75 year old woman with 4 episodes of "absence of vision"
Digital Journal of Ophthalmology 2002
Volume 8, Number 5
June 1, 2002
Volume 8, Number 5
June 1, 2002
PMHx: hypertension, hypothyroidism, oopherectomy, vein stripping (left lower extremity)
Meds: Vasotec, Synthroid, Premarin, Estrogen
SHx: Non contributory
FHx: Non contributory
- Pupils: Normal OU, No APD
- Color plates: 10/10 OU
- Motility: Full OU
- Intraocular pressures: Normal OU
- Slit lamp examination: normal anterior segments OU
- + Palpable temporal artery pulses OU
- Goldman visual fields: full fields OU
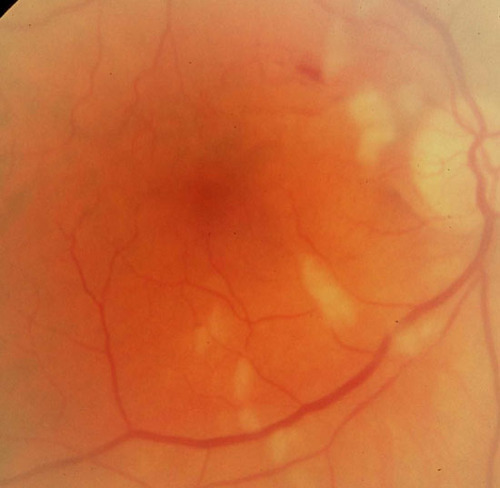
Figure 1
Multiple cotton wool spots are present along the vascular arcades and disc with intratretinal hemorrhages in the macula. The arteries are attenuated
Multiple cotton wool spots are present along the vascular arcades and disc with intratretinal hemorrhages in the macula. The arteries are attenuated
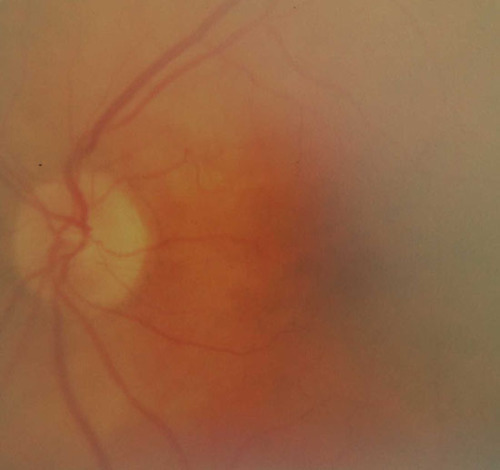
Figure 2
The arteries are slightly attenuated.
The arteries are slightly attenuated.
Blood work:
ESR 89
CRP 3.8 (0.0-0.5)
WBC 11. 1, Hct 32.8, Plt 528 (130-400)
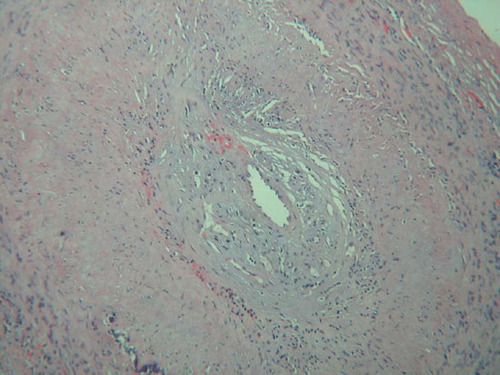
Figure 3
Histology demonstrates chronic vascultitis characterized by granulomatous and epitheliod inflammation in the media and adventitia.
Histology demonstrates chronic vascultitis characterized by granulomatous and epitheliod inflammation in the media and adventitia.
Giant cell arteritis (GCA) is a systemic disease that affects patients over the age of 55 years. Caucasian patients are most commonly affected; it is very uncommon in patients of African descent. Giant cell arteritis predominantly involves medium sized blood vessels of the cranium, heart, and eye. The pattern of arterial involvement is directly proportional to the amount of elastic tissue found in the media and adventitia. The posterior ciliary artery and temporal artery are rich in elastic tissue, hence their high incidence of involvement. Interestingly, the cranial vessels are protected FROM this inflammatory disease once they penetrate the dura mater.
Typical complications of untreated disease include blindness, stroke, and death secondary to ischemia. Ocular manifestations include anterior ischemic optic neuropathy (AION), central retinal artery occlusion, and (less commonly) cranial nerve palsies. Most commonly patients present with severe and permanent visual loss in one eye. Transient visual symptoms may occur in advance or permanent blindness. The second eye usually becomes blind in days to weeks if the disease is not treated appropriately.
A recent study by Hayreh et al revealed that jaw claudication, neck pain, erythrocyte sedimentation rate (ESR) of 47-107mm/hr, and C-reactive protein (CRP) above 2.45mg/dl are highly correlated with a positive temporal artery biopsy. A CRP is the most sensitive serologic test - it is 100% sensitive, compared to a sensitivity of 92% for the ESR. They also SHOW that ESR and CRP together provide the best specificity (97% specific) for the serologic diagnosis. However, the definitive diagnosis is achieved by a positive temporal artery biopsy.
A positive temporal artery biopsy shows evidence of chronic vasculitis characterized by granulomatous or epitheliod inflammation. Giant cells may or may not be seen. There is focal destruction of the internal elastical lamina, but this is a nonspecific sign that is seen as the result of aging alone. Temporal artery biopsy is 100% specific and 65-95% sensitive for the GCA. To address the variability in sensitivity, recent literature has discussed the diagnostic yield of bilateral biopsies. Three recent publications , , found the diagnosis on the two sides to be discordant in 1-5% of retrospective case reviews.
Occult giant cell arteritis is ocular involvement by GCA without any systemic symptoms. A recent prospective study by Hayreh et al showed the incidence to be 21.2%, with no influence by age or sex of the individual. The majority of ocular ischemia was AION (94.4%), and less commonly, central retinal artery occlusion (5.6%). The values of ESR and CRP are generally lower in this patient population.
Treatment is with oral prednisolone or high-dose intravenous methylprednisolone, dependent on the severity or extent of involvement. Side effects of prolonged steroid use include osteoporosis, increase in total body fat, and increase in glucose levels. We recommend a starting dose of at least 80mg per day of prednisone. Higher doses (1gram of methylprednisolone per day) can be used if the threat of ischemia is more severe.
Hayreh SS, Podhajsky PA, Raman R, et al. Giant cell arteritis: validity and reliability of various diagnostic criteria. Am J Ophthalmol 1997 March; 123(3):285-296.
Boyev LR, Miller NR, Green WR. Efficacy of unilateral versus bilateral temporal artery biopsies for the diagnosis of giant cell arteritis. Am J Ophthalmol 1999 August; 128(2):211-215.
Danesh-Meyer HV, Savino PJ, Eagle RC Jr, et al. Low diagnostic yield with second biopsies in suspected giant cell arteritis. J Neuroophthalmol 2000 September; 20(3):213-215.
Pless M, Rizzo JF III, Lamkin JC et al. Concordance of bilateral temporal artery biopsy in giant cell arteritis. J Neuroophthalmol 2000 September; 20(3): 216-218.
Hayreh SS, Podhajsky PA, Zimmerman B. Occult giant cell arteritis: ocular manifestations. Am J Ophthalmol 1998