63 year old woman with red eye
Digital Journal of Ophthalmology 2002
Volume 8, Number 6
July 1, 2002
Volume 8, Number 6
July 1, 2002
She re-presented to her outside ophthalmologist with worsening OD photophobia, redness, tearing, blurry vision, and pain. Corneal sensation was noted to be absent OD but intact OS. The xam was notable for eyelids without vesicles, conjunctival injection, corneal epithelial irregularity with small defect, mild corneal edema, keratic precipitates, and mild anterior chamber reaction.
A pressumptive diagnosis of herpes simplex virus (HSV) keratouveitis was made, and she was started on oral acyclovir (800mg 5x/day). Initially her symptoms improved slightly, but 1 week later she developed worsening corneal edema and anterior chamber reaction. Pred Forte was added TID resulting in reduced corneal edema and anterior chamber reaction. However, two weeks later, she developed worsening photophobia and pain.
She presented to the Massachusetts Eye and Ear Infirmary for a second opinion.
Previous ocular history: Myopia (rigid gas permeable contact lenses x 40 years)
Past Medical History: Chicken pox as a child
Medications: none
Family and Social History: non-contributory
Pupils: Normal (OU), no APD
Motility: Full (OU)
Tonometry: Normal (OU)
Corneal sensation: Absent OD
Slit Lamp Examination: Normal (OU)
Fundus Examination: Normal OU
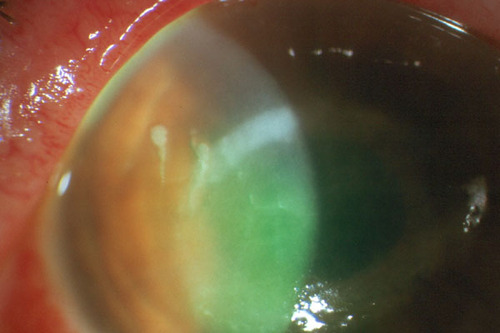
Figure 1a
Figures 1a-1c. Examination demonstrates corneal- ring infiltrate, central epithelial defect, stromal edema,
Descemet's folds, and keratic precipitates
Figures 1a-1c. Examination demonstrates corneal- ring infiltrate, central epithelial defect, stromal edema,
Descemet's folds, and keratic precipitates
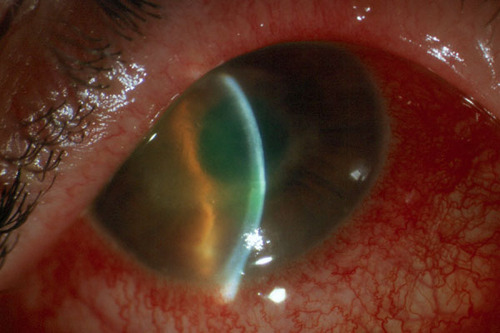
Figure 1b
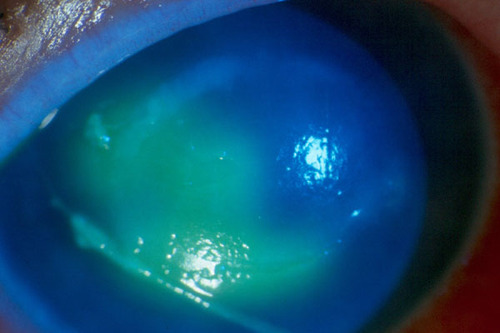
Figure 1c
- Viral keratitis (HSV and others)
- Bacterial keratitis
- Fungal keratitis
- Anesthetic abuse
Diagnostic studies:
- Bacterial cultures: negative
- Viral cultures: negative
- HSV PCR: negative
- Fungal cultures: negative
- Gram stain: PMNs, epithelial cells, no organisms
- Calcofluor white stain: negative
- Corneal biopsy: negative
- Acanthamoeba culture: positive
Risk factors for developing acanthmoeba keratitis include contact lens wear, use of homemade saline, exposure to contaminated water, and corneal trauma.Over 80% of cases are related to contact lens use. All lens types have been implicated, including soft, hard, gas-permeable, disposable, extended wear
Innoculation occurs through corneal epithelial breaks. Early infection involves the epithelium only followed by spread to all layers of corneal as well as nerves.The trophozoite produces cytolytic enzymes that aid in tissue invasion, loss of keratocytes, and stromal necrosis
Innate immunity plays an important role in figting acanthamoeba infection (Hurt M, Alizadeh H et al. Infect Immun 2001 69(5):2988-2995). In an animal model of Acanthamoeba keratitis, exacerbation of keratitis occurred when neutrophil migration was inhibited, and resolution of keratitis occurred when neutrophils were recruited. Adaptive immunity may also play a role, as anti-Acanthamoeba IgA antibodies have been demonstrated in tears (Niederkorn JY et al. Cornea 2001 20(6):622-627).
Symptoms are usually unilateral, and often include ocular pain out of proportion to exam, redness, decreased visual acuity, foreign body sensation, photophobia , and protracted progressive course with no therapeutic response to topical antimicrobial agents.
Many corneal manifestations may occur, including elevated epithelial lines that may form dendritic lesions, epithelial erosions, decreased corneal sensation, a gray-white ring infiltrate, nummular infiltrates, radial keratoneuritis, satellite lesions, disciform edema, thinning, land ack of neovascularization.Other signs may include follicular conjunctivitis, tender preauricular node, iritis, and lid abnormalities (edema, pseudoptosis).
Diagnostic modalities include culture, Giemsa Stain, corneal biopsy stained with Calcofluor White, confocal microscopy to detect organisms in vivo, and PCR (which is more sensitive than culture).
Early initiation of treatment is most effective and typically requires long-term therapy. Reported treatment modalities include epithelial debridement, diamidine derivatives (brolene, pentamidine), imidazole derivatives (miconazole, clotrimazole, ketoconazole), aminoglycosides (neosporin, paromycin) and cationic antiseptics (PHMB, chlorhexidine diacetate). Controversial therapies include penetrating keratoplasty, steroids, and cryotherapy. Limited clinical trial DATA exist to determine best treatment, as the incidence of this disease is low.