A 27-year-old man with traumatic partial dislocation of an intraocular lens
Digital Journal of Ophthalmology 2016
Volume 22, Number 1
February 2, 2016
DOI: 10.5693/djo.03.2015.10.003
Volume 22, Number 1
February 2, 2016
DOI: 10.5693/djo.03.2015.10.003
Download PDF
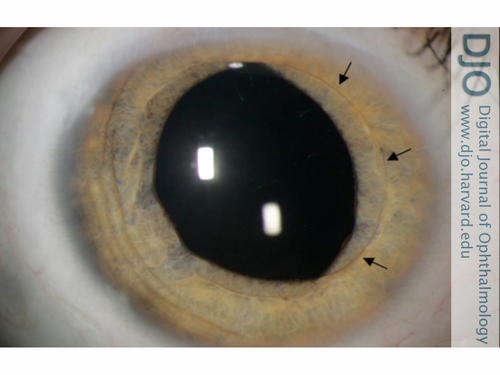
Figure 1
Partial pupillary capture of the intraocular lens (IOL). Arrows indicate the edges of the anteriorly dislocated optic.
Partial pupillary capture of the intraocular lens (IOL). Arrows indicate the edges of the anteriorly dislocated optic.
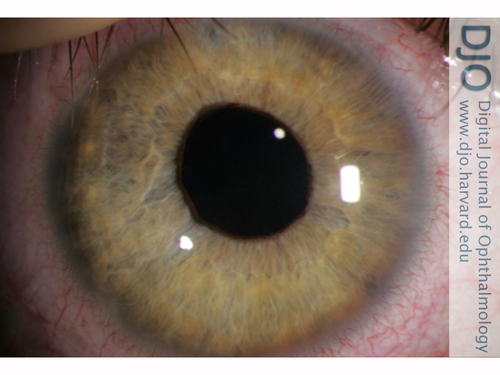
Figure 2
IOL repositioned after dilation with 10% phenylephrine and supine positioning for 6 hours.
IOL repositioned after dilation with 10% phenylephrine and supine positioning for 6 hours.
Galvis et al described a case of complete pupillary capture of an IOL after routine dilation with uncomplicated extracapsular cataract extraction 6 years previously.(6) After unsuccessful relocation with simple dilation, the IOL was successfully relocated with complete dilation and lens manipulation by applying corneal pressure with a three mirror lens and subsequent pupil constriction. Bowman et al reported a patient presenting with blurry vision and partial pupillary capture of an inferior optic that repositioned into the plane of the ciliary sulcus after gentle digital percussion on the temporal side of the patient’s closed lid.(7)
Other cases of surgical treatment for anterior dislocation of the IOL have been reported with an unremarkable recovery.(8) Superstein and Gans reported a case of traumatic anterior dislocation of a posterior chamber IOL in an 85-year-old man leading to reduction of visual acuity to hand motions and hyphema.(9) The dislocated IOL was exchanged for an anterior chamber IOL, with improvement of visual acuity to 20/40.
Nd:YAG laser photodisruption has also been described as a method for IOL relocation. For optics that are sufficiently mobile, the pressure wave created by the laser shifts the IOL back into position. Steinert and Puliafito reported a case of a posterior chamber IOL that dislocated anteriorly with routine pupillary dilation.(10) Redilation and mechanical manipulation were unsuccessful at relocating the optic. A 6 mJ pulse from an Nd:YAG laser applied to the peripheral edge of the IOL created pressure anteriorly that pushed the optic posteriorly behind the pupillary sphincter. Bartholomew reported 8 successful relocations of posterior chamber IOLs using Nd:YAG in 12 attempted treatments.(11)
In the present case a traumatic partial dislocation of a posterior chamber IOL with pupillary capture was successfully relocated with simple dilation and supine positioning. We recommend attempting this approach first in uncomplicated cases to avoid surgical, laser, or external lens manipulation treatment. If this technique is unsuccessful, pupil dilation with external manipulation may be indicated. If external manipulation fails, laser or surgical therapy can be considered.
Financial support
University of Minnesota, Minneapolis, Minnesota; Research to Prevent Blindness (RPB), New York, NY.
2. Bucci FA Jr, Lindstrom RL. Total pupillary capture with a foldable silicone intraocular lens. Ophthalmic Surg 1991;22:414-5.
3. Marcus DM, Azar D, Boerner C, Hunter DG. Pupillary capture of a flexible silicone posterior chamber intraocular lens. Arch Ophthalmol 1992;110:609.
4. Nagamoto S, Kohzuka T, Nagamoto T. Pupillary block after pupillary capture of an AcrySof intraocular lens. J Cataract Refract Surg 1998;24:1271-4.
5. Lavin M, Jagger J. Pathogenesis of pupillary capture after posterior chamber intraocular lens implantation. Br J Ophthalmol 1986;70:886-9.
6. Galvis V, Tello A, Montezuma S. Delayed pupillary capture and noninvasive repositioning of a posterior chamber intraocular lens after pupil dilation. J Cataract Refract Surg 2002;28:1876-9.
7. Bowman CB, Hansen SO, Olson RJ. Noninvasive repositioning of a posterior chamber intraocular lens following pupillary capture. J Cataract Refract Surg 1991;17:843-7.
8. Leccisotti, Antonio. Traumatic pupillary capture of the haptic of an angle-supported phakic intraocular lens. J Cataract Refract Surg 2006;32:2133-4.
9. Superstein R, Gans M. Anterior dislocation of a posterior chamber intraocular lens after blunt trauma. J Cataract Refract Surg 1999;25:1418-9.
10. Steinert RF, Puliafito CA. The Nd:YAG Laser in Ophthalmology: Principles and Clinical Applications of Photodisruption. Philadelphia, PA: Elsevier, 1985.
11. Bartholomew, R.S. Incidence, causes, and neodymium:YAG laser treatment of pupillarycapture. J Cataract Refract Surg 1997;23:1404-8.