An 82-year-old man with binocular oblique diplopia
Digital Journal of Ophthalmology 2015
Volume 21, Number 3
September 12, 2015
DOI: 10.5693/djo.03.2015.05.003
Volume 21, Number 3
September 12, 2015
DOI: 10.5693/djo.03.2015.05.003
Download PDF
Video 1
Sensorimotor examination revealing right hypertropia, right inferior oblique overaction and complete abduction palsy of the left eye.
Sensorimotor examination revealing right hypertropia, right inferior oblique overaction and complete abduction palsy of the left eye.
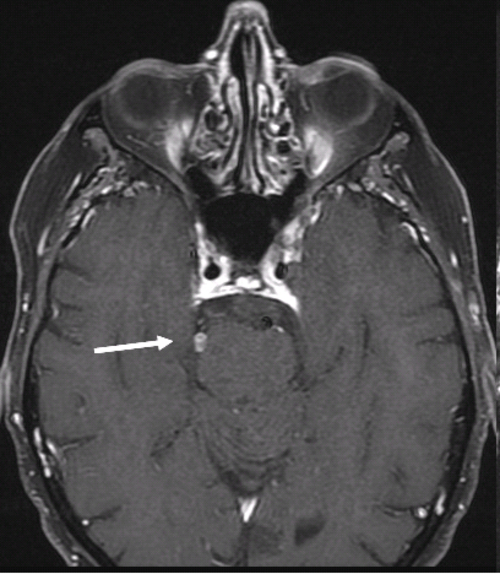
Figure 1
Axial T1 postcontrast image revealing an enhancing lesion in the right ambient cistern along the course of the right trochlear nerve (white arrow) consistent with right fourth nerve schwannoma.
Axial T1 postcontrast image revealing an enhancing lesion in the right ambient cistern along the course of the right trochlear nerve (white arrow) consistent with right fourth nerve schwannoma.
Figure 2
Thin-section axial FIESTA image revealing left sixth nerve compression by an anterior inferior cerebellar artery aneurysm (black arrowhead). The cisternal segment of the normal sixth nerve is seen on the right (black arrow).
Thin-section axial FIESTA image revealing left sixth nerve compression by an anterior inferior cerebellar artery aneurysm (black arrowhead). The cisternal segment of the normal sixth nerve is seen on the right (black arrow).
Acquired trochlear nerve palsies are most commonly secondary to head trauma, followed by microvascular ischemia and compressive lesions. They are much less commonly due to intrinsic neoplasms of the trochlear nerve.(1) Trochlear nerve schwannomas are extremely rare in patients without neurofibromatosis. The first case of trochlear schwannoma was described by King in 1976,(2) and fewer than 50 cases have since been reported in the literature. Patients may be asymptomatic or present with loss of function of the affected cranial nerve. Larger tumors may cause mass effect on adjacent cranial nerves or present with symptoms of brainstem compression.(1) MRI is useful for both diagnosis and follow-up of these lesions, which appear well demarcated, lie along the course of the nerve, and show homogenous enhancement.(3) Patients may be managed conservatively with serial scans; surgical intervention may be reserved for patients exhibiting signs of brainstem compression.(1)
Abducens nerve palsy is most commonly related to microvascular ischemia. The incidence of abducens nerve palsy associated with intracranial aneurysms is less than 4%.(4) Mechanisms by which an aneurysm may cause abducens nerve dysfunction include direct compression and an irritant effect of subarachnoid blood from rupture. Neurovascular compression of the abducens nerve may also result from dolichoectatic vertebral or basilar arteries, which may compress the nerve close to the root.(4,5) Compression of the nerve in the prepontine cistern from an AICA aneurysm has rarely been described. Thin section MRI using CISS/FIESTA sequence is the imaging modality of choice for evaluating neurovascular compression of the abducens nerve.(5) Aneurysms causing ophthalmoplegia may be treated by endovascular coiling although, especially in older patients and patients with microvascular risk factors, this treatment does not usually result in complete resolution of nerve palsy, and there may often be residual diplopia, especially in upward or downward gaze.(4,6)
Literature Search
The authors searched PubMed on July 27, 2014, for English-language articles (1950-present) using the following search terms: diplopia, trochlear schwannoma, anterior inferior cerebellar artery aneurysm, fourth nerve palsy, trochlear palsy, abducens palsy, sixth nerve palsy.
2. King JS. Trochlear nerve sheath tumor: case report. J Neurosurg 1976;44:245-7.
3. Gentry L, Mehta R, Appen R, Weinstein J. MR imaging of primary trochlear nerve neoplasms. Am J Neuroradiol 1991;12:707-13.
4. Ohtsuka K, Sone A, Igarashi Y, Akiba H, Sakata M. Vascular compressive abducens nerve palsy disclosed by magnetic resonance imaging. Am J Ophthalmol 1996;122:416-9.
5. Giray S, Pelit A, Kizilkilic O, Karatas M. Isolated abducens nerve palsy caused by contralateral vertebral artery dolichoectasia. Neurol India 2005;53:246-7.
6. Stiebel-Kalish H, Maimon S, Amsalem J, Erlich R, Kalish Y, Rappaport HZ. Evolution of oculomotor nerve paresis after endovascular coiling of posterior communicating artery aneurysms: a neuro-ophthalmological perspective. Neurosurg 2003;53:1268-73.