A 15-year-old girl with variable anisocoria
Digital Journal of Ophthalmology 2014
Volume 20, Number 1
January 12, 2014
DOI: 10.5693/djo.03.2013.10.001
Volume 20, Number 1
January 12, 2014
DOI: 10.5693/djo.03.2013.10.001
Download PDF
The patient provided several photographs that illustrate fluctuating symptoms. Figure 1 shows inappropriate dilation on a bright sunny day compared to other pictures of her on similar days; there is also subtle anisocoria greater in the right eye than in the left; either pupil could be involved during symptomatic episodes.
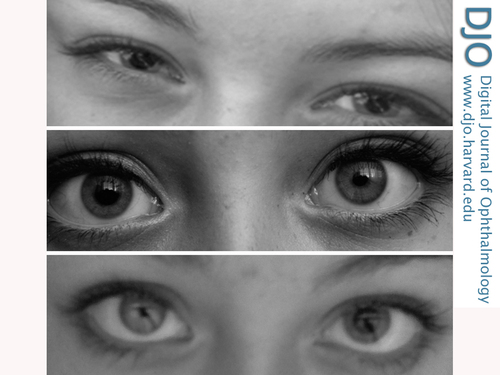
Figure 1
Photographs demonstrating the variable anisocoria. A, Bilateral mydriasis on a sunny day. B, Right-sided mydriasis. C, Left-sided mydriasis.
Photographs demonstrating the variable anisocoria. A, Bilateral mydriasis on a sunny day. B, Right-sided mydriasis. C, Left-sided mydriasis.
Three weeks later she was reexamined because of a worsening of her symptoms. On follow-up examination, her pupils were 8 mm and nonreactive to light, accommodation, or 1% pilocarpine. Distance visual acuity was 20/20 with correction and near acuity was J7 with correction and J2 without correction.
This case is remarkable in that the patient had variable and fluctuating pupillary dilation and accommodative failure. The initial hypersensitivity response to 0.125% pilocarpine was consistent with Adie’s tonic pupil but in the absence of other signs of this condition. Although we do not know the exact mechanism of the suprasensitivity response to 0.125% pilocarpine, it is tempting to consider that it was related to repeated, variable receptor blockade of the cholinergic receptor by glycopyrrolate.
Primary hyperhidrosis (axillary or palmar) is a disease of excessive sweating. Hyperhidrosis affects about 2.8% of the American population (7.8 million people), with axillary hyperhidrosis being the most prevalent manifestation.(9) The treatment options for hyperhidrosis include antiperspirants, oral or topical anticholinergics, and surgical or chemical (ie, botox injection) sympathecotomy.(10-13)
This case demonstrates the value of a careful history in dealing with patients with anisocoria and the need to ask specifically about hyperhidrosis and the use of glycopyrrolate whenever pharmacologic mydriasis is suspected.
2. Jacobson DM. Benign episodic unilateral mydriasis: clinical characteristics. Ophthalmology 1995;102:1623-7.
3. Evans RW, Jacobson DM. Transient anisocoria in a migraineur. Headache 2003;43:416-8.
4. Camkurt MA, Ay D, Akkucuk H, Ozcan H, Kunt MM. Pharmacologic unilateral mydriasis due to nebulized ipratropium bromide. Am J Emerg Med 2011;29:576.e5-6.
5. Panting KJ, Alkali AS, Newman WD, Sharpe GR. Dilated pupils caused by topical glycopyrrolate for hyperhidrosis. Br J Dermatol 2008;158:187-8.
6. Polomský M, Smereck J. Unilateral mydriasis due to hemorrhoidal ointment. J Emerg Med 2012;43:e11-5.
7. Wilhelm H, Wilhelm B, Schiefer U. Mydriasis caused by plant contact [in German]. Fortschr Ophthalm 1991;88:588-91.
8. Rubinfeld RS, Currie JN. Accidental mydriasis form blue nightshade “lipstick.” J Clin Neuroophthalmol 1987;7:34-7.
9. Strutton DR, Kowalski JW, Glaser DA, Stang PE. US prevalence of hyperhidrosis and impact on individuals with axillary hyperhidrosis: results from a national survey. J Am Acad Dermatol 2004;51:241-8.
10. Eisenach JH, Atkinson JL, Fealey RD. Hyperhidrosis: evolving therapies for a well-established phenomenon. Mayo Clin Proc 2005;80:657-66.
11. Izadi S, Choudhary A, Newman W. Mydriasis and accommodative failure from exposure to topical glycopyrrolate used in hyperhidrosis. J Neuroophthalmol 2006;26:232-3.
12. Collin J, Whatling P. Treating hyperhidrosis. Surgery and botulinum toxin are treatments of choice in severe cases. BMJ 2000;320:1221-2.
13. Vergilis-Kalner IJ. Same-patient prospective comparison of botox versus dysport for the treatment of primary axillary hyperhidrosis and review of literature. J Drugs Dermatol 2011;10:1013-5.