A 66-year-old woman with extensive conjunctival melanosis
Digital Journal of Ophthalmology 2014
Volume 20, Number 2
May 8, 2014
DOI: 10.5693/djo.03.2013.12.002
Volume 20, Number 2
May 8, 2014
DOI: 10.5693/djo.03.2013.12.002
Ocular adnexal examination was unremarkable. Slit-lamp examination revealed diffuse pigmentation of the bulbar conjunctiva nearly 360-degrees, with denser pigment superiorly. There was an area of raised conjunctiva superiorly. Pigment did not extend to the palpebral conjunctiva (Figures 1-2). Lids, lashes, cornea, and anterior chambers were unremarkable bilaterally.
Both pupils were pharmacologically dilated. Posterior chamber intraocular lenses were clear and well-positioned in each eye. Fundus examination revealed unremarkable maculae, vessels, and periphery in both eyes. Given the very asymmetric intraocular pressure measurements in the two eyes, the possibility of a trauma-induced, small, self-sealing scleral rupture was considered; nevertheless, given the intact anterior chamber and the extent of abnormal conjunctival pigmentation, a conjunctival biopsy was scheduled.
Two weeks later the patient returned for a scheduled biopsy of the conjunctiva. At this time, examination revealed a corectopic pupil with a peak at 12 o’clock (Figure 3). The conjunctiva was elevated superiorly overlying the area of iris prolapse (Figure 4). Conjunctival pigmentation was present and unchanged from initial examination.
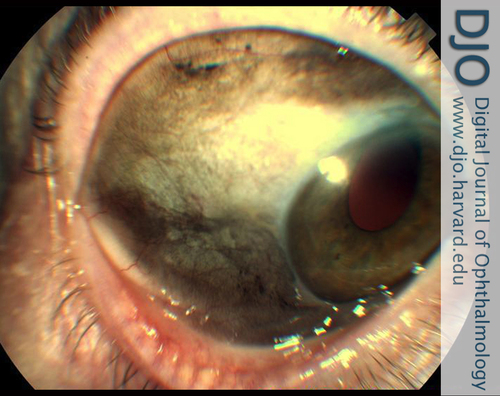
Figure 1
Temporal bulbar conjunctiva with diffuse pigmentation in the patient’s right eye at initial presentation.
Temporal bulbar conjunctiva with diffuse pigmentation in the patient’s right eye at initial presentation.

Figure 2
Magnified inferotemporal conjunctiva demonstrating lack of palpebral conjunctival pigment on initial presentation.
Magnified inferotemporal conjunctiva demonstrating lack of palpebral conjunctival pigment on initial presentation.

Figure 3
Pupil peak at 12 o’clock on repeat evaluation, 2 weeks following initial presentation.
Pupil peak at 12 o’clock on repeat evaluation, 2 weeks following initial presentation.

Figure 4
Superior conjunctiva showing iris prolapse with overlying conjunctival pigmentation on repeat evaluation, 2 weeks following initial presentation.
Superior conjunctiva showing iris prolapse with overlying conjunctival pigmentation on repeat evaluation, 2 weeks following initial presentation.
The differential diagnosis for pigmentation of the conjunctiva includes several etiologies, as previously mentioned, however new-onset conjunctival pigmentation that is rapidly progressive narrows the top of the differential to acquired melanosis (primary or secondary) and pigmented malignant neoplasia.
Conjunctival melanomas represent about 2% of all ocular malignancies and typically present as focal areas of raised macules, plaques, or masses in an asymptomatic patient, most commonly in the sixth decade.(7,8) Clinical features that may suggest conjunctival melanoma include large size, lack of mobility, limbal location, variegation, and presence of feeder vessels.(8) Conjunctival melanoma may arise from areas of primary acquired melanosis, de novo, or from a conjunctival nevus. Usually melanoma arising from a prior nevus or de novo, appears as black or grey vascularized nodule, whereas lesions arising from PAM with atypia have areas of nodularity and thickening. Conjunctival melanoma can also present as an amelanotic lesion with a pink, smooth “fish-flesh” appearance.(9) Whereas our patient demonstrated large areas of new conjunctival pigmentation, the history was significant for recent blunt trauma to the eye. Additionally, histological examination our patient’s conjunctiva confirmed that the deposition of pigment cells was not in the epithelial layer but rather deeper within the subepithelial layer and substantia propria.
Our patient’s medical history may have predisposed her to scleral perforation after blunt trauma. First, she has a history of cataract extraction performed through a superior scleral tunnel incision. Expulsive iridodialysis secondary to trauma has been noted in several case reports as a rare complication of blunt trauma to eyes that have undergone previous cataract surgery.(10-13) Second, our patient suffers from rheumatoid arthritis. Because there is an association between scleral thinning and perilimbal scleromalacia, she may have additionally been predisposed to scleral perforation after blunt trauma.(14,15)
Several case reports describe secondary acquired conjunctival melanosis after ocular trauma or surgery including intrableb pigmentation (IBP) after trabeculecomy and phacoemulsification,(2,3) pigmentation following pars-plana vitrectomy,(4) and pigmentation attributable to a surgical clamp.(5)
A similar case report by Benson et al describes centrifugal pigment dispersion diffusely throughout the conjunctiva following traumatic scleral perforation with iris incarceration.(6) Electron microscopy of conjunctival tissue from this case revealed many pigment-laden cells in the conjunctival substantia propria closely resembling the melanosomes found in the normal posterior iris pigmented epithelium. Presumably the incarcerated iris in both our case and this published case led to dispersion of iris pigment from mechanical forces rapidly into the conjunctiva.
Our patient’s rapid development of secondary acquired conjunctival pigmentation was a direct result of a perforating scleral injury with uveal tissue prolapse, and although uncommon, should be considered in the differential diagnosis for melanosis after trauma.
Acknowledgments
The authors wish to thank Walter Beebe, MD, and Dr. Robert Nick Hogan, MD, PhD, for their collaboration on case history, photographs, and histopathology.
2. Wanichwecharungruang B, Narumitchai W. Intra-bleb pigmentation after trabeculectomy. J Med Assoc Thai 2003;86:183-90.
3. Rebolleda G, Muñoz-Negrete FJ. Intra-bleb pigmentation after phacoemulsification [in Spanish]. Arch Soc Esp Oftalmol 2001;76:571-4.
4. Smiddy WE, Yeo JH, Michels RG, Green WR. Conjunctival pigmentation following pars plana vitrectomy. Retina 1987 Spring;7:38-40.
5. Campinchi R, Coscas G, Hamard H. A case of pseudo-melanosis of the conjunctiva caused by a surgical clamp [in French]. Bull Soc Ophtalmol Fr 1965;65:298-9.
6. Benson MT, Rennie I, Talbot J. External ocular pigmentation secondary to perforating eye injury. Br J Ophthalmol 1990;74:251-3.
7. Kanski JJ, Bowling B. Clinical Ophthalmology: A Systematic Approach. 7th ed. Philadelphia: Elsevier/Saunders; 2011:482-3.
8. Zembowicz A, Mandal R, Choopong P. Melanocytic lesions of the conjunctiva. Arch Pathol Lab Med 2010;134:1785-92.
9. Skuta GL, Cantor LB, Weiss JS. Ophthalmic Pathology and Intraocular Tumor, Basic and Clinical Science Course. San Francisco: The American Academy of Ophthalmology; 2009:70-1.
10. Zurutuza A, Andonegui J, Berástegui L. Traumatic expulsive iridodialysis with vitreous prolapse. Int Ophthalmol 2011;31:469-70.
11. Navon SE. Expulsive iridodialysis: an isolated injury after phacoemulsification. J Cataract Refract Surg 1997;23:805-7.
12. Walker NJ, Foster A, Apel AJ. Traumatic expulsive iridodialysis after small-incision sutureless cataract surgery. J Cataract Refract Surg 2004;30:2223-4.
13. Kloek CE, Andreoli MT, Andreoli CM. Characteristics of traumatic wound dehiscence. Am J Ophthalmol 2011; 152:229-33.
14. Cappin JM, Allen DW. Paralimbic scleromalacia. Spontaneous scleral intercalary perforation. Br J Ophthalmol 1973;57:871-2.
15. Chan AY, Liu DT. A case of Behcet’s disease with scleromalacia perforans. Rheumatology (Oxford). 2005 Aug;44(8):1077; author reply 1077-8.